Recurrent Respiratory Papillomatosis (RRP) also known as juvenile-onset laryngeal papillomatosis/ laryngeal papillomatosis, is a rare airway disease characterized by the development of small, wart-like growths (papillomas) anywhere in the respiratory tract anywhere from the nasal vestibule to a terminal bronchiole.
The papillomas predominantly arise at areas where a change in epithelium happens – these areas are the tonsillar pillars, uvula, vocal folds, and laryngeal commissure.
There are two subdivisions of this clinical condition.
- adult-onset recurrent respiratory papillomatosis (AORRP) and
- juvenile-onset recurrent respiratory papillomatosis (JORRP)
Etiology
Southern blot tests have identified the Human Papilloma Virus (HPV) as a causative organism for RRP. HPV subtypes 6, 11 and rarely 16 are associated with the recurrent respiratory papillomatosis.
HPV enters traumatized epithelium, reside in the basal layer of the mucous membrane, where it replicates by a process known as episomal maintenance. This affects normal cell maturation, epithelial proliferation, and neovascularization.
Epidemiology
RRP has got a bimodal age distribution – the juvenile variant has an onset peak at 3-4 years while adult variant peaks at 20-30 years.
Sex ratios are almost the same with both boys and girls are equally affected. The condition is severe in children than in adults.
The estimated prevalence rate of JORRP is 4 per 1lakh children. It is the commonest benign laryngeal neoplasm in children and the second most common cause for childhood hoarseness.
JORRP is thought to be caused by the acquisition of HPV during passage through the birth canal of an infected mother. The classical triad associated with JORRP patient is a young mother with genital warts, with prolonged vaginal delivery from low social-economic status. Usually, the disease affects the first child because of the prolonged second stage labor. But this relation is not scientifically proved as only 1in 400 children born to infected mothers have the disease, which may be because of the host factors.
It is estimated that approximately 5% of the U.S. population may have HPV in their respiratory tract, but less than 1 in 1000 of those infected ever develop RRP. Hence it is considered that some subtle immunologic alterations (like HLA polymorphism) affect the respiratory tracts of those few who develop RRP. HLA polymorphism (HLA DRB1*0301) is found to be a factor causing severe disease because of reduced interferon-gamma expression.
Clinical presentation
The most common region of airway affected is the larynx, and the patient presents with hoarseness, breathiness, stridor (inspiratory or biphasic), chronic cough, paroxysms of chocking, recurrent respiratory infections, occasional respiratory distress, aphonia, and failure to thrive.
JORRP is typically diagnosed between the ages of two and three years, and most children are diagnosed before five years of age. But some children may be misdiagnosed for asthma, laryngitis, bronchitis or croup and delay for diagnosis of JORPP can happen up to 8 years.
Diagnosis
Recurrent Respiratory Papillomatosis is typically diagnosed by an ear, nose and throat physician (ENT) performing an examination of the larynx.
Stridor in any children warrants an endoscopy. An awake fiberoptic naso-pharyngo-laryngoscopy, with 2.2mm endoscopes, under IV sedation, or inhalation with spontaneous respiration should be carried out to know the reason for stridor.
Helical CT is the imaging modality of choice for further evaluation of RRP when extra-laryngeal spread is suspected and can be considered prior to pulmonary referral.
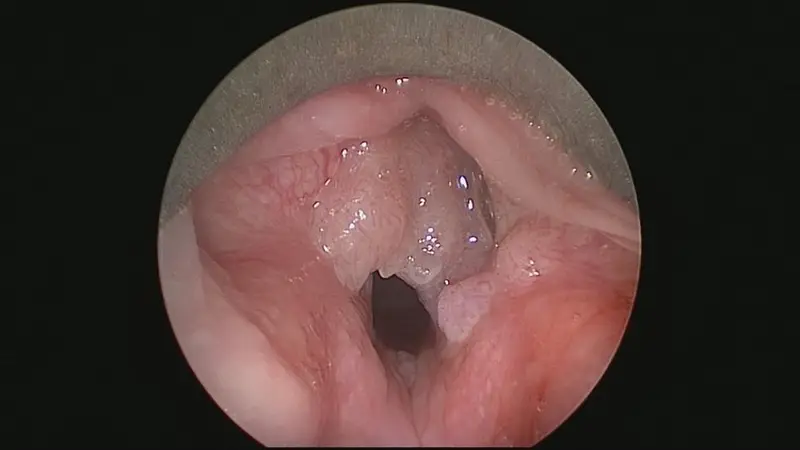
Physical examination typically reveals multiple verrucous, polypoid, non-friable growths, either pedunculated or sessile lesions which, spread over the mucosal surface of the larynx and trachea.
Histologically they appear as exophytic projections of keratinized squamous epithelium overlying a fibrovascular core, with varying degrees of dyskeratosis, parakeratosis, and dysplasia. Koilocytosis (vacuolated cells with clear cytoplasmic inclusions) is often seen indicating viral infections.
Viral typing by PCR is needed, which may help to predict the aggressiveness of the lesions. Usually, severe disease is strongly associated with HPV 11.
Staging of Recurrent Respiratory Papillomatosis
Derkay staging system is the most common and popular staging system for Recurrent Respiratory Papillomatosis.

The operating surgeon assigns a score of 0 to 3 (0 = absent, 1 = surface lesion, 2 = raised lesion, and 3 = bulky lesion) to each site in the aerodigestive tract involved. A composite score is generated by summing the scores at each involved site. The scoring system needs the surgeon to answer six questions regarding the patient’s clinical course. A clinical score is generated by summing the scores for each of the subjective assessments.
In addition to the questionnaire, the surgeon denotes the laryngeal lesions on a standardized diagram, indicates sites of biopsy and laser treatment, documents sites in which adjuvant drug therapy has been administered.
Course and Natural History
The course and natural history of the disease are extremely variable, with some patients having spontaneous remission.
In JORRP poor prognostic signs include the onset of disease before age of three, birth by cesarean section and low socioeconomic status. But current evidence does not support Caesarean section as prophylaxis against JORRP.
Surgical debridement for maintaining an airway is the mainstay of treatment. Most children need serial debulking in 2-3months interval. Severe disease may need weakly debulking. The median number of debulking needed in a patient is reported as 7-13. But repeated debulking can cause glottic scarring, webbing which leads to voice changes.
Remission is seen in early teenage years which is thought to be due to hormonal changes only, not because of clearance of HPV from the mucosa.
Surgical treatment for RRP
As mentioned above, the aim of management in RRP is maintaining an airway, preventing tracheostomy, and giving the patient a serviceable voice.
The primary treatment modality is surgery, and the following are surgical options are available for the treatment of RRP.
Powered debrider: Powered debrider is the gold standard for papilloma removal in the larynx. This approach is extremely precise with minimal mucosal damage and with minimal bleeding. Unlike other approaches like a laser, there is no risk of thermal injury or laser plumes.
Studies have shown good disease clearance, fewer hospital stays and less post-operative pain with the use of powered instruments.
Cold steel surgery: like a powered instrument, cold steel technique also has the advantage of no thermal injury or laser plumes exposure. In addition, the use of a micro flap technique minimizes trauma to vocal folds with satisfying disease clearance. Lack of direct hemostasis is a disadvantage of the cold steel technique.
Laser – CO2, KTP, ND: YAG and PULSED-DYE Laser: Laser provides the ability to ablate papilloma with minimal bleeding, minimal vocal fold fibrosis and consequently minimal voice damage.
In addition to the risk of thermal damage, laser injury and plume exposure, some late complications like vocal fold fibrosis, inter arytenoid fibrosis and stenosis, glottic webbing, arytenoid fixation etc. are reported with the use of a laser.
Photodynamic therapy: In this treatment option, photosensitizing agents like Di-hematoporphyrin Ether (DHE) or meso-tetra-hydroxyphenyl chlorin (mTHPC), etc. are injected intravenously prior to laser surgery. Rapidly proliferating tissues selectively take up these photosensitizing agents. These agents release tumoricidal oxygen derivatives when activated by laser light of appropriate wavelength.
The main disadvantage is that the patient remains photosensitive for six to nine months and may experience skin erythema, blistering and ocular discomfort.
Tracheostomy: Role of tracheostomy in RRP is controversial. This is because tracheostomy will create a new squamociliary junction at the stoma site. This site may present an additional area of predilection for papillomas. Tracheostomy is performed in papillomatosis as a life-saving procedure only.
In addition to surgical treatment, some adjuvant medications are used as adjuvant treatment for RRP. These drugs can be broadly classified into antiviral groups and antiproliferative/immunomodulatory groups. As of 2019, at the time of this publication, there are no consensus recommendations met regarding intralesional adjuvant therapies.
Interferon-α: Interferons are naturally produced by human leukocytes. Pharmaceutically they are prepared by recombinant DNA technology. Interferon- α have antiviral, anti-proliferative and immunomodulatory properties.
By depleting essential metabolites in papilloma cells, they increase the length of their multiplication cycle, thereby slowing target cell growths. Interferon-α also helps in the recognition of papilloma cells by circulating antigens by enhancing expressions of cell surface antigens.
The recommended dosage is 2-5MU/m2 of body surface area.
Some side effects reported with usage of interferons are constitutional symptoms like fever, generalized flu-like symptoms, nausea, and vomiting, hematological problems like pancytopenia, hepatorenal failure, cardiac dysfunction, rebound phenomenon associated with withdrawal, etc.
Pegylated interferon alfa-2a, usually called peginterferon, is a chemically modified form of the standard interferon and has a better safety profile.
Cidofovir: Cidofovir is an acyclic nucleoside phosphonate that is active against a broad spectrum of DNA viruses including HPV. The drug acts by inhibition of viral DNA polymerases essential for viral replication.
Intralesional injections are given in JORRP at a dosage of 1mg/ml two weekly intervals for four treatments and then the interval is extended by one week after each and
every subsequent treatment. Some surgeons consider concomitant laser debulking also. In 2012, a Cochrane review identified a single randomized controlled trial of intralesional cidofovir in RRP that did not demonstrate benefit; however, the dosage administered in this study was substantially lower than typically utilized.
The systemic use of Cidofovir is associated with neutropenia and nephrotoxicity.
Ribavirin: Is a synthetic nucleoside that has activity against a broad spectrum of viruses. The drug is principally used as an aerosol in the treatment of human respiratory syncytial (RSV) associated pneumonia and Hep C.
Anecdotal evidence has shown some benefit of this drug as an adjuvant in the treatment of JORRP.
Acyclovir: is a nucleoside analog antiviral drug that inhibits thymidine kinase present in Herpes Simplex Virus (HSV) but not in HPV. This way the drug eradicates HSV and thus removes its synergism with HPV. As of now evidence of acyclovir for the treatment of RRP is weak in literature.
Indole 3 Carbinol: This is derived from brassica family vegetables – Cabbage, Broccoli, Brussels. The drug is a Cytochrome p450 enzyme inducer. Though it has been found to be a successful treatment option for JORRP it’s efficacy in pediatric patients needs further study.
Estrogen hormone increases HPV expression and allows epithelial cell proliferation. Cytochrome p450 enzyme inducer regulates estrogen metabolism, shifting production of antiproliferative estrogen and alter the growth pattern of RRP invitro.
Cimetidine: is a Histamine (H2) antagonist drug with an immunomodulatory effect at higher doses (40mg/kg for four months). This immunomodulatory effect is used in the treatment of RRP.
Bevacizumab: is a monoclonal antibody against vascular endothelial growth factor A (VEGF‐A), used in the treatment of JORRP. Studies have shown a 90% reduction in recurrence after 5 cycles of treatment. While there are no RCTs to date, published data have been promising and without significant side effects.
In addition to surgery and the adjuvant treatment, effective control of gastroesophageal reflux disease (GERD) is also needed for better symptom control. A short course of anti-reflux measures is usually advised in the post-operative period to reduce reflux.
Providers that practice in high-risk populations may consider evaluation for other infectious diseases (e.g., human immunodeficiency virus, HIV; tuberculosis, TB) once the diagnosis of RRP is made. Referral to infectious disease may follow if indicated.
The use of quadrivalent HPV Vaccine, programmed cell death protein 1 (PD-1), celecoxib, heat shock protein, and gene therapy in prophylaxis and treatment of RRP are in early stages.
The parents/caretakers should be well educated regarding the disease, the prognosis, the need for multiple surgeries and information regarding support groups (e.g., the RRP Foundation).
Extralaryngeal Papillomatosis
Extralaryngeal spread occurs in around one-third of patients with recurrent respiratory papillomatosis.
Tracheal involvement may appear as cobblestoning of mucosa coupled with the presence of papillomas. Presence of subglottic papillomas, presence of a tracheostomy and a longer duration of disease are the factors predisposing for tracheal spread.
More distant obstructions in bronchi may cause obstructive pneumonia. Pulmonary papilloma initially begins as asymptomatic non-calcified peripheral nodules. Lesions eventually enlarge, finally become central cavitation and liquefactive necrosis with air-fluid levels on CT scan.
Extralaryngeal papillomas have very poor prognosis and malignant degeneration can happen in such cases.
Malignant transformation of Papillomas
Malignant transformation of respiratory papillomas is a rare complication, but with a devastating sequel with the condition a universally fatal one.
Most incidences of malignant transformations are reported in adults associated with other risk factors including tobacco use, long-standing disease. In children, malignant transformation happens in the bronchopulmonary tree, while in adults it is in the larynx.
HPV 6 and 11 produces transforming oncoproteins E6 and E7, which causes inactivation of p53 and pRb tumor suppressor genes. E6 and E7 also affect cell cycle regulatory proteins. This causes the proliferation of cells and contributes to a malignant phenotype.
HPV 16 associated infection is more prone to malignant transformation than other viral types.
Another etiology for malignant transformation was the use of radiation as a treatment for RRP in older days. Radiotherapy is not a treatment option anymore and this etiology has got only historical relevance.
References
- Tasca RA, Clarke RW. Recurrent respiratory papillomatosis. Arch Dis Child 2006; 91:689.
- Armstrong LR, Derkay CS, Reeves WC. Initial results from the national registry for juvenile-onset recurrent respiratory papillomatosis. RRP Task Force. Arch Otolaryngol Head Neck Surg 1999; 125:743.
- Shah KV, Stern WF, Shah FK, et al. Risk factors for juvenile onset recurrent respiratory papillomatosis. Pediatr Infect Dis J 1998; 17:372.
- Kashima HK, Shah F, Lyles A, et al. A comparison of risk factors in juvenile-onset and adult-onset recurrent respiratory papillomatosis. Laryngoscope 1992; 102:9.
- Quick CA, Watts SL, Krzyzek RA, Faras AJ. Relationship between condylomata and laryngeal papillomata. Clinical and molecular virological evidence. Ann Otol Rhinol Laryngol 1980; 89:467.
- Parsons DS, Bothwell MR. Powered instrument papilloma excision: an alternative to laser therapy for recurrent respiratory papilloma. Laryngoscope 2001; 111:1494.
- Derkay CS, Wiatrak B. Recurrent respiratory papillomatosis: a review. Laryngoscope 2008; 118:1236.
- Chadha NK, James A. Adjuvant antiviral therapy for recurrent respiratory papillomatosis. Cochrane Database Syst Rev 2012; 12:CD005053.
- Sidell DR, Nassar M, Cotton RT, et al. High-dose sublesional bevacizumab (avastin) for pediatric recurrent respiratory papillomatosis. Ann Otol Rhinol Laryngol 2014; 123:214.
- DeMarcantonio M., Derkay C. (2013) Laryngeal Papillomatosis. In: Kountakis S.E. (eds) Encyclopedia of Otolaryngology, Head and Neck Surgery. Springer, Berlin, Heidelberg