Papillary carcinoma thyroid (PTC) is the most common differentiated malignancy of thyroid gland. Depending on the different histopathological patterns, cell types and clinical features different variants of papillary carcinoma thyroid have been described.
Knowing the variants of papillary carcinoma thyroid can help in predicting the aggressive biological course and prognosis of the disease. This, in turn, allows surgeons and endocrinologists to formulate a more complete treatment plan, including total thyroidectomy, possible lymphadenectomy, and postoperative radioiodine administration.
About 50% of PTC are of the conventional subtype, while the other 50% is made up of less common histologic variants.
For diagnosis of all variants of papillary carcinoma, except oncocytic and hobnail, microscopically it should have more than 50% of tumors showing their unique patterns along with nuclear features. Oncocytic variant should show the morphology in more than or equal to 75% while hobnail variant should have hobnailed nuclei in more than or equal to 30%.
Several studies have demonstrated a poorer prognosis for specific subtypes of papillary thyroid cancers, including tall cell, insular, and hobnail variants.
Patients with rare variants of papillary carcinoma thyroid need to be managed more aggressively than are those with classical papillary cancer of the same stage.
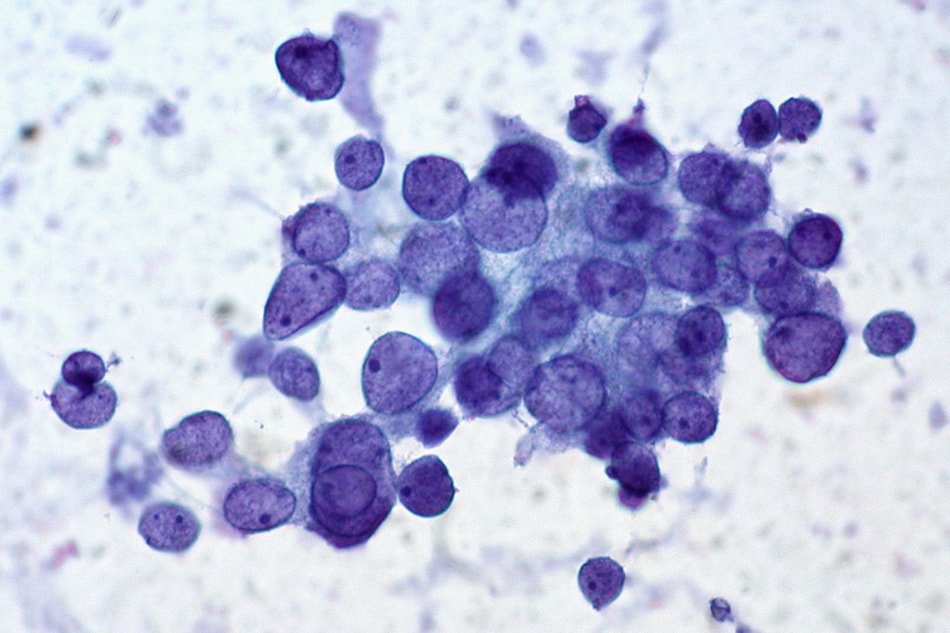
Histopathological photographs of the variants of carcinoma thyroid can be found in this article.
Conventional Papillary Carcinoma Thyroid
- Conventional PTC has an excellent prognosis.
- Microscopically
- shows a papillary architecture with branching.
- papillae are covered by cells with eosinophilic cytoplasm and enlarged nuclei.
- “Psamomma bodies” with concentric lamellae composed partly of thyroglobulin are more common in approximately 50% of papillary carcinoma thyroid. These are the scarred remnants of tumor papillae that presumably infarcted.
- tumor cells containing large, oval, crowded and overlapping nuclei with nuclear clearing (“Orphan Annie cells”) and nuclear grooves and nuclear membrane irregularities.
- Some tumors may show squamous metaplasia, and some may contain multinucleated giant cells also.
- Shows a BRAF mutation more often (35–70%)
Tall Cell Variant
- Seen more commonly in the elderly.
- Accounts for 10% of cases.
- Present with large bulky tumors which are usually larger and aggressive than conventional PCT.
- An extra-thyroidal extension is more common.
- Microscopically, the cells are 2–3 times as tall as they are wide and show cytologic features of papillary thyroid carcinoma.
- Tumor cells have abundant eosinophilic cytoplasm, necrosis, mitotic activity and nuclear features similar to conventional papillary carcinoma.
- These tumors typically associated with a V600E mutation in the BRAF gene.
- Less sensitive to radioiodine ablation
- The 10-year survival rate is 70%.
- These tumors have more chance of recurrence.
Follicular variant
- A unique variant of PTC with different genetic profile.
- Grossly looks like follicular neoplasm.
- Microscopically shows darker or hyper eosinophilic colloid, with occasional multinucleated giant cells within the follicles.
- Often diagnosed as follicular neoplasm in fine needle cytology.
- Subcategorized into
- a noninvasive, encapsulated, well-circumscribed subtype (NI-FVPTC) – frequently have the RAS mutations.
- an invasive subtype with either invasion (capsular or vascular invasion) or lacking a well-defined capsule (diffuse/multinodular) – often harbor BRAF V600E mutations.
- Prognosis similar to conventional PTC except for diffuse-type which have an aggressive course.
- Because of the better prognosis and non-invasive nature, NI-FVPTC is renamed as noninvasive follicular thyroid neoplasm with papillary-like nuclear features (NIFT-P tumors).
Diffuse Sclerosing Variant
- More common in young age group, between 15 and 30 years of age
- Characterized by diffuse involvement of the thyroid with both lobes typically involved.
- Microscopically show extensive squamous metaplasia, abundant psammoma bodies, stromal fibrosis and prominent lymphocytic infiltration (thyroiditis picture)
- Clinically aggressive tumor, but with better prognosis
- Almost all cases show lymph node metastasis at the time of initial presentation.
- Lung metastasis is seen in 25% of cases at the time of presentation.
Columnar Cell Variant
- A rare variant of PCT
- Microscopically shows pseudostratified columnar cells with supranuclear and subnuclear cytoplasmic vacuoles resembling endometrial or colonic adenocarcinomas.
- More aggressive than the typical PTC
- Low incidence of metastasis
Solid / Trabecular cell variant
- More common in children with a history of radiation exposure
- Microscopically shows sheets of tumor cells, which have cytological features of conventional PTC – mimics a solid type of poorly differentiated carcinoma.
- One-third of cases show vascular invasion and extrathyroidal extension.
Cribriform morular variant
- Rare variant
- Typically associated with familial adenomatous polyposis and Gardner Syndrome (APC Mutations).
- Usually multifocal
- Microscopically shows a cribriform pattern, solid and spindle cell areas with squamous morule.
Clear cell variant
- Microscopically comprised of mainly clear cells having a papillary architecture and cytological features of PTC
- Immunostaining for TTF-1 and thyroglobulin may be necessary to distinguish these tumors from a clear cell carcinoma of other organs such as the kidney or colon that have metastasized to the thyroid.
Hobnail variant
- Clinically very aggressive carcinomas associated with mortality of almost 50%
- Microscopically had more than 30% of the tumor with hobnail features
Oncocytic / Warthin variant
- Clinically aggressive
- Resistant to radioiodine therapy
- Grossly tumor have a distinct brown color similar to the follicular Hurthle cell tumors.
- Microscopically may have follicular or papillary architecture.
- The “Warthin-like” oncocytic variant has abundant lymphocytic stromal infiltrate and is often seen with Hashimoto’s thyroiditis.
Papillary microcarcinoma
- This is not a specific variant but includes all PTC which are usually found incidentally and measure less than 1 cm in diameter.
- These tumors are also called “incidentaloma” as they are usually detected during investigations for any other illness.
- Seen often close to the capsule and are frequently non-encapsulated.
- Non-encapsulated, those with extensive sclerosis and having BRAF mutations are more aggressive with comparatively poor prognosis.
Other rare variants of papillary carcinoma thyroid
- Hurthle / Oxyphilic variant: – cellular features of Hürthle cell carcinomas but cells that are arranged in papillary formations.
- Papillary Thyroid Carcinoma with Fasciitis-like Stroma:- rare variants of PTC associated with fasciitis like stroma or fibromatosis-like stroma, which mimics PTC with de-differentiation to anaplastic carcinoma.
- Combined Papillary Thyroid Carcinoma and Medullary Thyroid Carcinoma:- consists of separate areas or cells with PTC or medullary thyroid carcinoma
- Papillary Thyroid Carcinoma with Dedifferentiation to Anaplastic Carcinoma: – PTC can undergo dedifferentiation or transformation to anaplastic carcinoma.
References
- Lloyd, R. V., Buehler, D., & Khanafshar, E. (2011). Papillary thyroid carcinoma variants. Head and neck pathology, 5(1), 51–56. doi:10.1007/s12105-010-0236-9
- Sak SD. Variants of papillary thyroid carcinoma: multiple faces of a familiar tumor. Turk Patoloji Derg 2015;31:34-47