Meniere’s Disease (Ménière’s Disease) is a disorder of the inner ear characterized by a triad of severe dizziness (vertigo), ringing sensation in the ears (tinnitus) and fluctuating hearing loss, with a feeling of fullness or congestion in the ear.
Epidemiology
- The disease most commonly affects females than males.
- Mostly in middle age/ elderly.
- Incidence 15/1 lakh population and prevalence of 220/1 lakh.
- 10% of patients who visits vestibular clinic are diagnosed with Meniere’s.
- The National Institute on Deafness and Other Communication Disorders (NIDCD) estimates that approximately 615,000 individuals in the United States are currently diagnosed with Meniere’s disease and that 45,500 cases are newly diagnosed each year.
Pathology
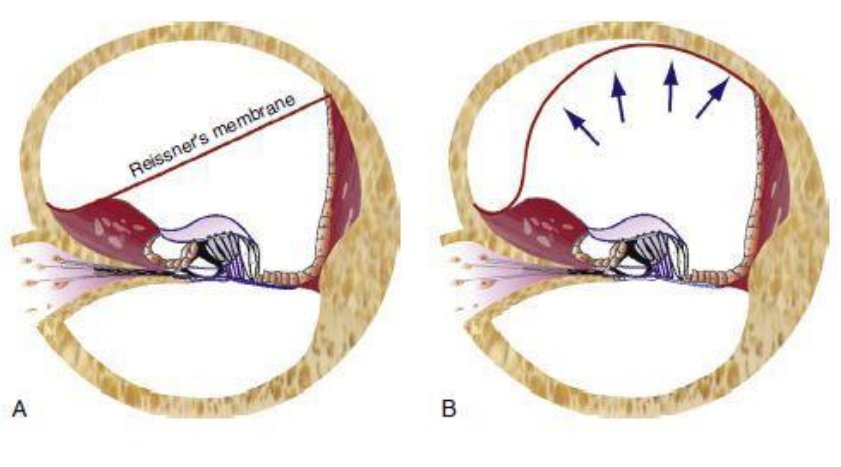
- Main pathology of Meniere’s disease is distension of endolymphatic system, mainly cochlear duct (Scala media) and saccule, and to a lesser extend utricle and semicircular canals.
- There is marked distension of cochlear duct, with bulging of Reissner’s membrane, completely filling Scala vestibuli.
- The distended saccule lies against stapes foot plate.
- The distended utricle and saccule show outpouchings into semicircular canals.
Meniere’s Attack
- Attacks of dizziness may come on suddenly or after a short period of tinnitus or muffled hearing. Some people will have single attacks of dizziness separated by long periods of time. Others may experience many attacks closer together over a number of days.
- These attacks are due to periodic rupture of Reissner’s membrane (separating endolymph & perilymph) resulting in leakage of potassium rich endolymph into perilymph.
- A typical attack has 3 phases.
- Irritative phase
- Initial excitation of hair cells due to increased potassium concentration around their basal surfaces causes irritative phase.
- Nystagmus is usually horizontal, horizontal-torsional, beats towards affected ear.
- Usually lasts less than an hour.
- Paretic phase
- Due to result of blockade of neurotransmitter release
- Nystagmus beats away from affected side.
- Lasts less than an hour.
- Recovery phases
- In this phase, healing of the rupture causes restitution of normal chemical composition resulting in termination of attack and improvement in vestibular and auditory function.
- Irritative phase
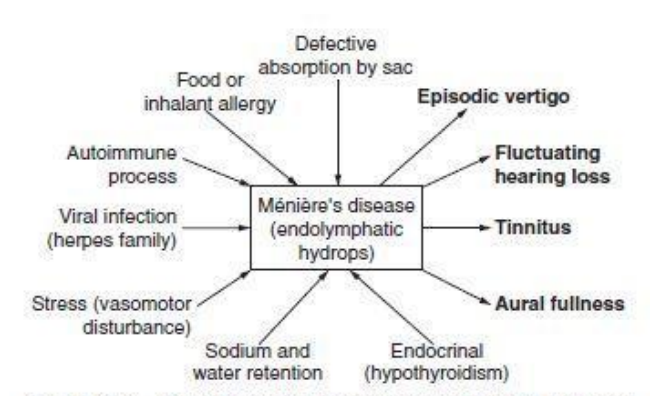
Etiology of Meniere’s disease
Many theories exist about what happens to cause Meniere’s disease, but no definite answers are available.
- Mostly idiopathic (unknown reasons).
- Infection – viral (mumps, measles), bacterial (syphilis, meningitis)
- Head trauma
- Endolymphatic hydrops
- Due to overproduction or malabsorption of endolymph causing gross enlargement of membranous labyrinth leading to hydrops.
- Normally endolymph is produced by stria vascularis, it fills the membranous labyrinth and is absorbed through endolymphatic sac. In some patients’ ischemic changes, which may limit re-absorption of endolymph, has been observed during sac surgeries.
- Autoimmunity – to inner ear antigens.
- Vasomotor disturbances
- Sympathetic over activity resulting in spasm of internal auditory artery and/or its branches interfering in function of cochlear or vestibular sensory epithelium.
- Anoxia of capillaries of Stria vascularis also causes increased permeability with transudation of fluid and increased production of endolymph.
- Allergy
- Offending allergen may be a foodstuff or an inhalant and inner ear acts as a shock organ.
- 50% of Meniere’s patient have a concomitant inhalant or food allergy.
- Hypothyroidism
- 3% of Meniere’s disease are due to hypothyroidism.
- Such patients get benefited from thyroid replacement therapy.
- Sodium and water retention
The final conclusion is that Meniere’s disease can be multifactorial with common endpoint of endolymphatic hydrops.
Clinical features of Meniere’s disease
- Mostly in age group 35-60years.
- Females affected more than males, mostly in middle age/ elderly.
- Mostly a unilateral condition, although bilateral Meniere’s seen in 2-7% cases.
Symptoms & Signs
- Characterized by a triad of Sensory neural hearing loss, Episodic vertigo and tinnitus.
- Deafness
- Patient will complaints of unilateral fluctuating hearing loss
- Usually accompanies vertigo or may precede it.
- Hearing loss may persist for days, improves during period of remission, deteriorates with each episode.
- Some may have diplacusis (hearing disorder whereby a single auditory stimulus is perceived as different pitches between ears).
- Audiometry will show sensory neural type of hearing loss (SNHL)
- During early days of Meniere’s, the audiogram will show as low frequencies affected more than higher (ascending type). But later become flat / sloping hearing loss.
- Some patients may show positive recruitment test.
- Episodic vertigo
- Occurs many years after unilateral hearing loss.
- Recurrent, well-defined episodes of true rotatory / spinning vertigo is the most disabling symptom – like being pulled to one side.
- Vertigo increases in intensity over a period of minutes and then lasting for about 30 minutes to several hours (even 24 hours)
- Autonomic symptoms like nausea, vomiting, anxiety, abdominal cramps, diarrhea, cold sweats and bradycardia during vertigo is common.
- Nystagmus will be present with attacks.
- There wont be any neurologic symptoms.
- Tinnitus
- Variable, often low pitched, roaring type and louder during attacks and may persist for days.
- The tinnitus is subjective type.
- Change in intensity and pitch of tinnitus may be a warning sign of an attack.
- Aural fullness
- Pressure sensation deep within ear which may accompany or preceed an attack of vertigo.
Variants of Meniere’s disease
- Lermoyez attack
- Symptoms of Meniere’s disease is seen in reverse order.
- Progressive deterioration of hearing, followed by attack of vertigo at which time hearing and tinnitus improves.
- Drop attacks / Tumarkin’s or Otolithic crisis.
- Seen in late stages of Meniere’s disease as a result of acute otolithic dysfunction.
- Patient simply falls to ground without warning and can sustain injuries.
- Sense of being pushed to ground by some external force.
- No associated vertigo or loss of consciousness.
- Cochlear Meniere’s *
- Hearing loss, Tinnitus, aural fullness with no vertigo in initial days.
- Vertigo appears after several years.
- The pathology is believed to be a block at level of ductus reuniens.
- Vestibular Meniere’s *
- Vestibular symptoms with no auditory symptoms in initial days.
- Cochlear symptoms appear later.
- In most of these cases endolymphatic hydrops couldn’t be demonstrated and are labelled as recurrent vestibulopathy.
- Delayed Endolymphatic Hydrops
- Arising of vestibular symptoms several years (usually 20) after a profound hearing loss in one ear.
- Etiology
- Proposed that Meniere’s disease may occur as a delayed sequel of inner ear damage sustained during an attack of subclinical viral labyrinthitis occurring in childhood.
- Clinical features
- May be ipsilateral or contralateral type.
- Ipsilateral type
- Patient has SNHL caused in childhood by head trauma, mumps, influenza or congenital anomalies.
- The patient develops severe, recurrent Meniere type vertigo.
- Contralateral type
- Fluctuating hearing loss, tinnitus, pressure and vertigo in opposite ear.
*Cochlear and Vestibular Meniere’s are now being abandoned in favor of AAO-HNS classification.
Differential Diagnosis / Meniere’s Syndrome/ Secondary Meniere’s syndrome
- Any inner ear or temporal bone diseases with similar clinical picture as that of Meniere’s disease can be a differential.
- Syphilis, Mumps, Cogan’s syndrome, Trauma, even chronic otitis media.
- Vestibular neuronitis – Single spontaneous vertigo lasts for hours to days. But usually there won’t be hearing loss.
- Migrainous vertigo – recurrent spontaneous attacks of vertigo, with no auditory symptoms and no permanent vestibular or auditory loss.
Diagnosis of Meniere’s disease
- Diagnosis of Meniere’s is purely clinical based on history and clinical features.
- Unilateral, low frequency SNHL with aural fullness, tinnitus and episodic vertigo lasting for few minutes to several hours.
- Otoscopy – Normal tympanic membrane
- Nystagmus – during acute attack, quick component is towards affected side.
- Tuning fork tests & audiometry – SNHL
| AAO-HNS criteria for diagnosis of Meniere’s disease. | |
| Major criteria | |
| Vertigo |
|
| Deafness |
|
| Tinnitus |
|
| Levels of certainty in diagnosis of Meniere’s | |
| Possible Meniere’s |
|
| Probable Meniere’s |
|
| Definite Meniere’s disease |
|
| Certain Meniere’s Disease |
|
Staging of Meniere’s
Done in certain and definite cases of Meniere’s disease.
Based on average of audiometry thresholds at 0.5, 1, 2 and 3KHz (rounded to nearest whole number) of the worst audiogram during six months interval before treatment.
| Stages | Pure tone audiometry average in dB in previous 6 months |
| Stage 1 | ≤ 25dB |
| Stage 2 | 26-40dB |
| Stage 3 | 41-70dB |
| Stage 4 | >70dB |
Assessment of severity of symptoms
- Jacobson’s Dizziness Handicap inventory (DHI) scale is the most commonly used questionnaire for assessment of severity of symptoms in Meniere’s disease.
- It consists of 25 questions pertaining to the physical, emotional and functional disability experienced by the patient due to vertigo.
- Each question contains three options, ‘no’ (worth 0 points), ‘sometimes’ (worth 2 points) or a ‘yes’ (worth 4 points) as it is answered by the patient.
- Each patient could, therefore, score between 0 and 100 points.
- The lower the score, the lesser the dizziness handicap.
Investigations
- Hennebert’s sign – False positive fistula test due to dilated saccule touching stapes foot plate – seen in 30% Meniere’s patients.
- Pure tone audiometry
- Fluctuating low frequency SNHL in early stages.
- Rising type of curve, later become flat or sloping.
- As disease progress, a permanent loss of hearing affecting all frequencies., resulting in flat SNHL.
- Speech audiometry
- Speech discrimination score (SDS) is usually between 55-85% between the attacks.
- SDS much impaired during and immediately after the attack.
- Special audiometry tests
- Recruitment test positive
- SISI – over 70%.
- Tone decay test – less than 25dB.
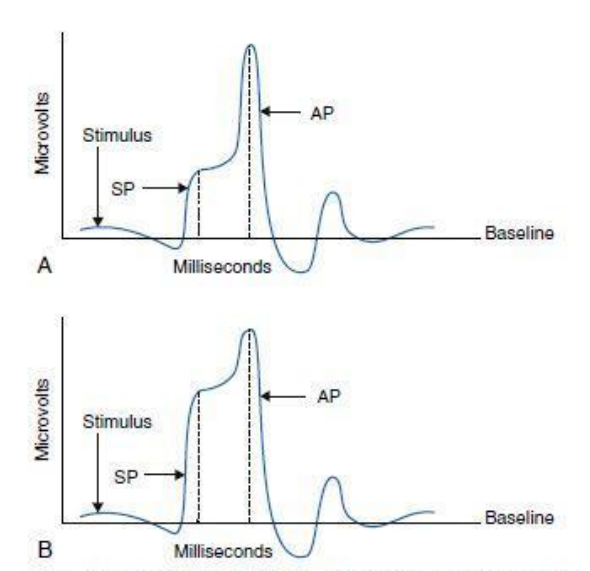
- Electrocochleography (ECoG)
- Most specific and sensitive for Meniere’s disease when tone-burst and click stimuli are used, and when responses are recorded trans-tympanically at promontory.
- Giving patients 4g of oral salt for three days prior to ECoG increases sensitivity of test.
- Normally ratio of summating potential to action potential is 30%; this ratio is higher in Meniere’s.
- Caloric test
- Reduced response in affected ear in 75% cases.
- Glycerol test
- Glycerol being a dehydrating agent, when given orally reduced endolymph pressure and causes improvement in hearing.
- Patient is given glycerol (1.5ml/kg) with an equal amount of water and a little flavoring agent or lemon juice.
- Audiogram and SDS are recorded before and 1-2hours after ingestion of glycerol.
- An improvement of 10dB in two or more adjacent octaves or gain of 10% in SDS makes a positive test.
- There is an improvement in tinnitus and aural fullness also.
- Test has both diagnostic and prognostic value.
- Gold standard – Autopsy histopathology of temporal bone.
- Idiopathic endolymphatic hydrops commonly affecting cochlea, saccule, utricle and semicircular canal’s (SCC) ampullae.
- Structural defects or holes in walls of membranous labyrinth covered by new membranes.
- Degenerative changes of sensory hair cells seen in advanced cases.
- Reduction in the number of afferent nerve endings and synapses in the cochlea.
- Significant loss of type II hair cells in all sensory regions of vestibular organ.
- Significant loss of vestibular ganglion cells.
- ABR
- To rule out retrocochlear pathologies.
Natural history of Meniere’s disease
Without treatment,
- 30% patients improve within 2 years and more than 70% in 8 years.
- 30% continue to have symptoms.
Management of Meniere’s disease
- No evidence based uniform treatment regimen exists for Meniere’s disease.
- General measures
- Reassurance
- To relieve patient anxiety by explaining true nature of disease.
- Diet
- Avoid excessive water intake.
- Strict sodium restriction to maximum of 1mg/1.5-2mg per day, so that urinary sodium is less than 50mMol/day.
- Salt restriction shown vertigo control in 79% and hearing improvement in 35% at a 2 year follow up.
- But no double blind RCT exists for its efficacy.
- Lifestyle changes
- Avoidance of alcohol caffeine, stress.
- Cessation of smoking.
- Avoid activities needing good body balance – like diving, flying or working in heights.
- Immunotherapy and food elimination.
- In patients with suspected allergy
- Management of acute phase
- Reassurance
- Bed rest with head supported on pillows to prevent excessive movements.
- Vestibular sedatives
- Dimenhydrinate (Dramamine)
- Promethazine (Avomine)
- Prochlorperazine (Stemetil)
- Diazepam (Valium or Campose) – 5 to 10mg iv has tranquillizing effect and also suppress activity of medial vestibular nucleus.
- Atropine 0.5mg subcutaneous useful in some patients.
- Vasodilators
- Carbogen inhalation – Carbogen is 95% CO2 with 5% O2, is a good cerebral vasodilator and improves labyrinthine circulation.
- Histamine drip
- Histamine diphosphate 2.75mg dissolved in 500ml of glucose, given as iv drip at a slow rate is a good vasodilator and helps to control acute attacks.
- Adverse effects: tachycardia, hypotension, hyperthermia and bronchospasm.
- Caution: should not be used on empty stomach.
- Contraindicated: Asthmatics
- Management of chronic phase
- Vestibular sedatives
- Prochlorperazine (Stemetil) 10mg three times daily, orally for 2 months and then reduced to 5mg thrice daily for another month.
- Diuretics
- May be effective in long-term control of vertigo but not for cochlear symptoms.
- Furosemide
- 40mg tablet on alternate days with potassium supplementation.
- Thiazides
- Bendrofluazide
- Reduces absorption of electrolytes from renal tubules, increasing excretion of sodium, chloride ions and water.
- No data on efficacy of treatment in Meniere’s.
- Side effects – hypokalemia, impotence.
- Patient needs potassium supplementation, potassium rich diets, monthly serum electrolyte assay.
- Chlorthalidone
- Sulphonamide derivative.
- Reported beneficial in some studies.
- Has teratogenic side effects.
- Acetazolamide
- Carbonic anhydrase inhibitor.
- Bendrofluazide
- Betahistine
- Tradenames – Vertin, Vertistar etc.
- Dosage 8/16mg thrice daily /twice daily given orally.
- Weak agonistic action of both H1 and H2 and moderate antagonistic action of H3 histamine receptors.
- Most drug trials suggested a reduction of vertigo with betahistine, but none of them were free of bias.
- Used as antivertigo measure in Meniere’s disease.
- Causes reduction of asymmetric functioning of vestibular end organs.
- Improves microvascular circulation in Stria vascularis of cochlea.
- Inhibition of activity in vestibular nuclei.
- Less specific effects on alertness through cerebral H1 receptors.
- Other drugs
- Nicotinic acid – 50mg taken about an hour before meals thrice a day.
- Causes vasodilatation.
- Dose can be increased slowly to achieve flushing of skin.
- Flunarizine, Cinnarizine
- No evidence to suggest that these are effective or more effective than betahistine.
- Hormones
- Replacement of thyroxine in patients with hypothyroidism.
- Propantheline Bromide (Probanthine)
- 15mg three times daily can be given alone or in combination with vasodilator is quite effective.
- Steroids
- Based on assumption of autoimmune pathogenesis of Meniere’s – provides immunosuppression.
- Suggested in cases of bilateral involvement and with coexistence of autoimmune symptoms/signs/elevated serum levels of autoantibodies.
- No double blinded randomized control trials to prove its clinical efficacy.
- Oral recommended treatments include high doses of prednisone for one month with slow tapering over 4-6months.
- Topical application via tympanotomy tubes achieves better drug penetration and fewer side effects than systemic administration.
- Studies have shown 35.4% improvement in hearing and 63.4% improvement in vertigo when treated with 16mg intratympanic and 16mg intravenous dexamethasone for 3 consecutive days, followed by oral dexamethasone.
- Nicotinic acid – 50mg taken about an hour before meals thrice a day.
- Vestibular sedatives
Surgical Treatment for Meniere’s disease
Surgery may be recommended when all other treatments have failed to relieve dizziness.
Aims of surgical treatment
- Abolish or alter function of labyrinth.
- Modification of underlying pathophysiology
- Altering production, distribution of endolymph or delivering steroids that may affect outcome of disease.
Selection of patients for surgery depends on various factors.
- Older age patients have more peri/post-operative complications associated including CSF leak.
- Status of contralateral ear
- Involvement of contralateral ear varies from 2-78%.
- Ablative therapy is appropriate for long standing unilateral Meniere’s disease when there is no clinical evidence of involvement of contralateral ear at time of therapy.
- Ablative surgery on one ear can limit the options of treatment in contralateral ear, once Meniere’s disease develops later in contralateral ear.
Limitations of surgical treatment
- Causes risk of hearing loss.
- Natural history of Meniere’s disease has shown 60-80% spontaneous remission of episodic vertigo – can confound surgical results.
Non-ablative procedures
- Intra tympanic injection of corticosteroids
- A ventilation tube is placed prior to initiation of therapy.
- Dexamethosone (2-24mg) is now standard therapy for control of vertigo in Meniere’s although repeat injections are frequently needed.
- Optimal drug frequency is unknown.
- Has an anti-inflammatory property, influences ion transport.
- Shows control in 80-96% early Meniere’s cases, but a subsequent RCT shown no benefit in later stages.
- Local overpressure therapy
- Here also a ventilation tube is placed prior to initiation of therapy.
- Application of external pressure to middle ear was reported to decrease Meniere’s symptoms in 4-5 patients during acute vertigo attacks.
- The mechanism of relief is unknown – supposed to be increased endolymphatic pressure facilitating its absorption.
- Meniett device – FDA approved in 2000, is a hand-held air pressure generator, that patient self-administers 3 times daily. The pressure is delivered in complex pulses of up to 20mm water over 5 minutes period.
- An RCT has shown improvement in first 3 months, but long-term results similar to natural history of Meniere’s.
- A mere placement of ventilation tube itself has shown control of vertigo in many patients.
- Cochlear implant
- Patients undergoing cochlear implant due to hearing loss in Meniere’s has found to have less vertigo following surgery.
Partial ablation
- Intra tympnanic Gentamicin (GM) / Chemical labyrinthectomy.
- High efficacy of controlling vertigo upto 90%.
- Reserved for vertigo control in patients with unilateral Meniere’s disease refractory to other treatment.
- Gentamicin is more vestibulotoxic than cochleotoxic – can control vestibular symptoms while sparing hearing.
- Gentamicin gains access to internal ear via round window membrane. The diffusion may be affected by increased thickness of round window membrane (Inflammation, Obstruction with fat / fibrous tissue).
- The concentration of Gentamicin reaching perilymph is 5-10% of that of that of applied solution and has elimination half-life of 75 minutes.
- When Gentamicin reaches endolymph, it is selectively concentrated in type I hair cells and supporting cells. These cells are destroyed by
- Blocking ion current through stereocilia.
- Causes adhesion of stereocilia.
- Destroys dark cells of secretory epithelium, thus decreasing endolymph production.
- Technique of intratympanic Gentamicin injection.
- Direct injection through tympanic membrane is the easiest method.
- Since multiple doses may be injected, a ventilation tube insertion is done initially.
- Prior to injection, tympanic membrane is anesthetized with topical application of 4% / 10% xylocaine and canal wall infiltration given with 2% xylocaine.
- Using a 25G needle, a superior port is made to allow air exit from middle ear and an inferior port for injection.
- Middle ear generally hold 0.5-0.8ml of fluid.
- After the injection, a brief episode of vertigo happens, which can be avoided by mildly warming the solution before injection.
- The patient is then instructed to lie straight in slight Trendelenburg position with treated ear up for 30 minutes, so that the bulk of injected drug concentrates at round window region and will not escape through eustachian tube.
- Single dose of Gentamicin is sufficient to markedly reduce vestibular function; 1/3rd of patients will need additional doses of Gentamicin.
- Current trend is to avoid multiple doses of Gentamicin . A single injection regimen with additional doses only if needed to control symptoms is recommended – Titration therapy.
- Disadvantages
- Profound SNHL in 3-30% cases.
- Hair cells may be able to self-repair after Gentamicin injection.
- Recurrence of vertigo in 29% cases within 24 months of treatment.
- Possibility of future bilateral involvement should be considered before any destructive procedure
- Endolymphatic sac decompression
- An active controversial topic.
- Theories
- External decompression of sac
- Neo-vascularization of perisaccular region.
- Passive diffusion of endolymph.
- Creation of an osmotic gradient out of semicircular canals.
- Procedure
- Cortical mastoidectomy done.
- Lateral and posterior canals skeletonized
- The landmark for superior aspect of sac is just below Donaldson’s line (formed by extending plane of LSCC posteriorly to bisect PSCC).
- Bone over posterior fossa removed completely between sigmoid sinus and vertical part of facial nerve.
- The sac lies medial to vertical segment of facial nerve and retrofacial cells.
- Variations
- Simple decompression, wide decompression including sigmoid sinus.
- Sacculotomy / Ficks operation
- Puncturing saccule with a needle through stapes footplate.
- Keeping a sharp prosthesis permanently through stapes footplate, which pierces sac when it expands.
- Otic-periotic shunt is a tube placed through round window membrane that perforates basilar membrane.
- Cochleo-sacculotomy – Cochlear duct is punctured and drained into perilymph by fracture dislocation of osseus spiral lamina.
- Cannulation of endolymphatic duct.
- Removal of extraosseous portion of sac.
- Drainage to subarachnoid space, mastoid.
- Endolymphatic mastoid shunting
- Paparella & Hanson technique – Incising the lateral wall of exposed sac and releasing any intraluminal adhesions, probing the duct and placing a stent to keep it open to mastoid cavity for long term.
- Endolymphatic subarachnoid shunting
- After initial lateral incision on sac, a small medial incision is made to allow silicone shunt to be passed into basal cistern.
- The CSF leak is controlled by placing a graft lateral to IAC and obliterating the mastoid cavity with fat.
- Complications of decompression and shunting
- 5% risk of hearing loss
- Damage to facial nerve.
- CSF leak
- Intracranial hematoma
- Selective Vestibular neurectomy
- Advantages
- Vestibular nerve section has complete vertigo control rate in 85-95% cases.
- 80-90% patient maintaining hearing postoperatively.
- Better results than sac decompression.
- Less chance of hearing loss than Gentamicin injection.
- Disadvantage
- Invasive and technically challenging.
- Approaches
- Retro sigmoid approach
- Retro sigmoid approach first described by Dandy in 1930.
- Provides enough exposure and direct view of VII, VIII nerves. Preferred method.
- Standard sub occipital craniotomy with sigmoid sinus as anterior limit of exposure – posterior fossa dura is opened – cerebellum is retracted to expose CP angle and petrous ridge – cistern is decompressed with an incision, and cerebellum is further retracted – vestibular nerve, cochlear nerve and facial nerve identified – Superior and Inferior vestibular nerve resected – Dura reapproximated – Bone flap repositioned and closed – Wound closed in layers.
- Middle cranial fossa (MCF) approach
- House in 1960
- Only minimal dural violation.
- Vertical incision above auricle – temporalis fascia freed from squamous portion of temporal bone – small craniotomy made in squamous portion of temporal bone – Middle cranial fossa dura elevated – using a Fisch or House urban retractor temporal lobe is elevated – Arcuate eminence and geniculate ganglion are identified in floor of middle cranial fossa as landmark for IAC – Using diamond burr IAC is unroofed – dissection carried out laterally to identify Bills bar which divides facial nerve (anteriorly) from superior vestibular nerve (posteriorly) – Dura of posterior part of canal is incised and superior vestibular nerve is identified – As superior vestibular nerve is retracted inferior vestibular nerve can also be identified – The nerves are sectioned, taking care not to injury cochlear nerve and internal auditory artery – IAC covered with fascia – bone flap repositioned – incision closed.
- Risk of facial nerve palsy palsy is higher in MCF than in sub occipital approach – rarely done these days.
- Sub occipital approach
- Retro labyrinthine approach
- Transmeatal cochleovestibular neurectomy.
- Retro sigmoid approach
- Advantages
Total ablation (Labyrinthectomy)
Most destructive procedure in treatment of Meniere’s disease, destroys both hearing and vestibular function.
- Ideal candidate for labyrinthectomy
- Patient with profound deafness
- Failed conservative management like gentamicin injection.
- Advantages
- Higher success rate in controlling vertigo than Vestibular neurectomy, 98% improvement in quality of life.
- Approaches
- Transcanal
- Middle ear exposed through tympanomeatal flap – Incus, Stapes removed to expose oval window – hook is inserted into vestibule to remove neural epithelium/ Promontory is drilled out to connect oval and round windows.
- Limitations
- Limited exposure – technically difficult.
- Poor access to posterior semi circular canal (PSCC) – failure to achieve complete ablation.
- Transmastoid
- Better exposure, more popular.
- Standard mastoidectomy is done – LSCC, SSCC, PSCC and facial nerve delineated – canals are then blue lined and followed medially to vestibule while removing neuroepithelium under direct vision.
- Advantages
- Allows direct visualization of vestibular end organ.
- Disadvantages
- Complete hearing loss – Some surgeons preserve hearing by packing SCC with bone wax and using a diamond burr to remove canal while preserving vestibule.
- Transcanal