
Thyroid nodules are extremely common with a reported prevalence ranging between 8.2% and 64.6% in autopsies and 19% to 68% in adults on high-resolution ultrasound. Most of the time, thyroid nodules are detected accidentally when neck imaging is done for some other reasons.
Mostly these nodules are benign; and even malignant nodules, particularly those smaller than 1 cm, regularly exhibit non-aggressive behavior or indolent course. Therefore, not all detected nodules require Fine Needle Aspiration (FNA) and/or surgery to reach a definitive diagnosis.
But in routine practice, many nodules are biopsied to identify the small percentage of malignant lesions.
In the United States, it is estimated that over diagnosis of thyroid cancer, defined as “diagnosis of thyroid tumors that would not, if left alone, result in symptoms or death” accounts for about 70% to 80% of thyroid cancer cases in women and 45% of cases in men between 2003 and 2007.
Hence, it is critical to know which nodules on thyroid ultrasound imaging need additional evaluation like FNA / surgery for definitive diagnosis of malignancy.
In order to address this dilemma, researchers have proposed multiple risk stratification systems called Thyroid Imaging Reporting and Data System (TI-RADS) based on the ultrasonographic characteristics, similar to the system used for breast lesions, (BI-RADS). These include.
- American College of Radiology: ACR TI-RADS
- European Thyroid Association: EU TI-RADS
- Korean Society of Thyroid Radiology: K TI-RADS
“American Thyroid Association guidelines for the assessment of thyroid nodules” and “Society of Radiologists in Ultrasound (SRU) guidelines for the assessment of thyroid nodules” are two other ultrasound-based risk stratification systems but not TI-RADS based.
Among these, the most popular and most commonly followed one is the ACR TI-RADS
ACR TI-RADS
In 2017, the American College of Radiology (ACR) presented a new risk-stratification system for classifying thyroid nodules on the basis of their appearance at ultrasonography. The paper provides recommendations for when to further evaluate the nodule with FNAC, a follow-up ultrasound examination or which nodules can be safely left alone, etc.
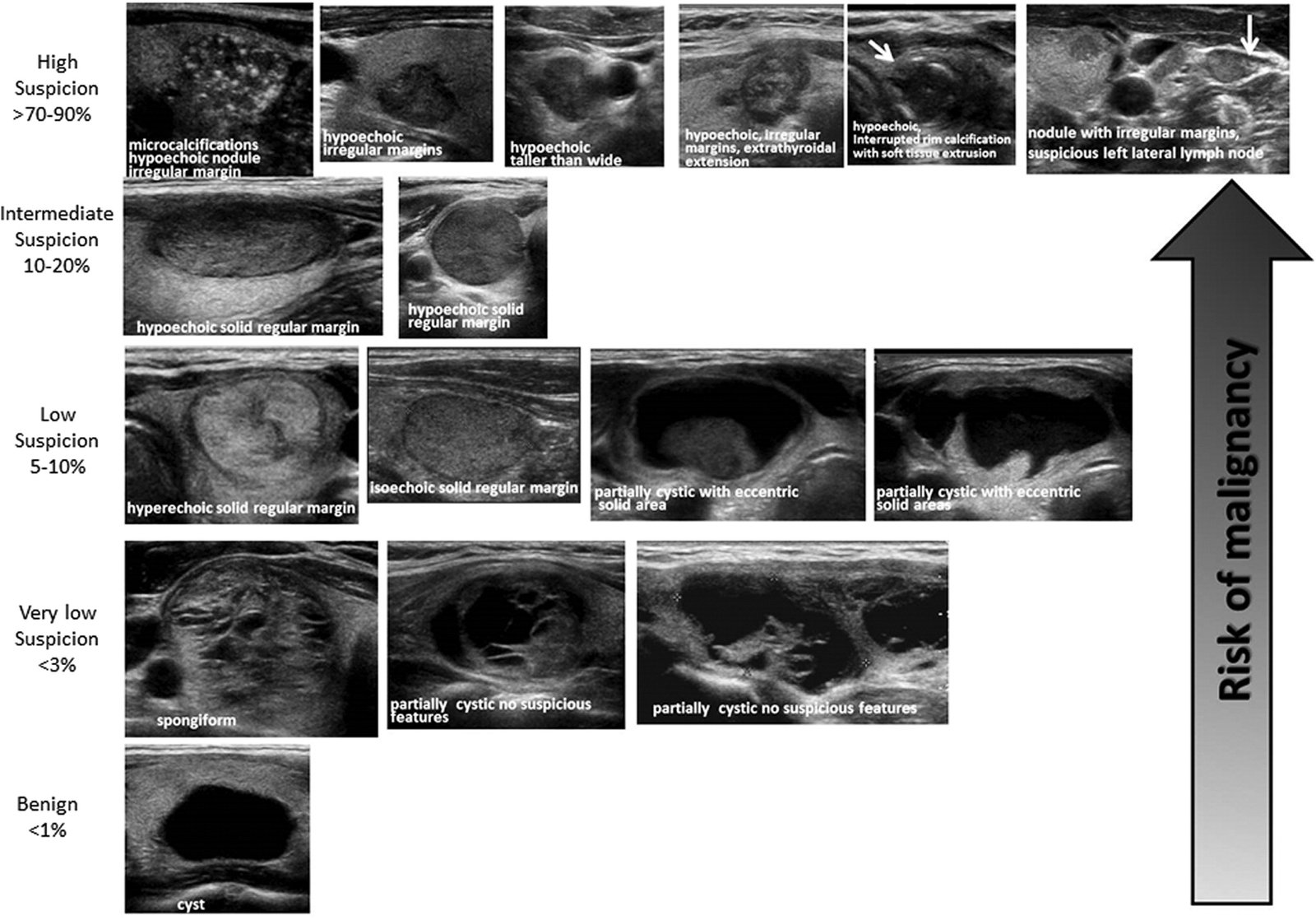
The ACR TI-RADS uses a standardized scoring system, based on five sonographic categories—composition, echogenicity, shape, margin, and echogenic foci—in which each feature is assigned 0–3 points.
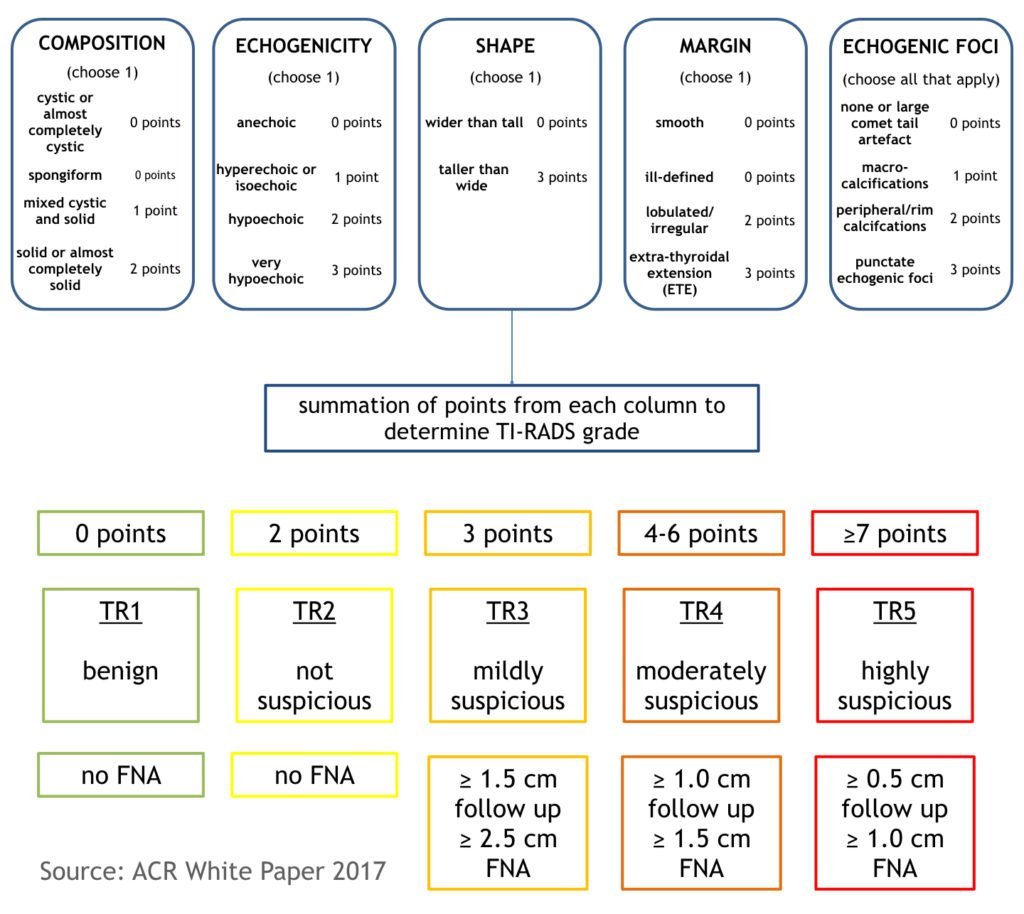
The nodule’s total point determines its risk level, which ranges from TR1 (benign) to TR5 (highly suspicious of malignancy).
| Total point | TR Score | Classification | Need for FNAC | Follow up | Risk of malignancy |
| 0 | TR1 | Benign | no FNAC required | 0.3% | |
| 2 | TR2 | Not suspicious | no FNAC required | 1.5% | |
| 3 | TR3 | Mildly suspicious | ≥1.5 cm follow up, ≥2.5 cm FNAC | 1, 3 and 5 years | 4.8% |
| 4-6 | TR4 | Moderately suspicious | ≥1.0 cm follow up, ≥1.5 cm FNAC | 1, 2, 3 and 5 years | 9.1% |
| ≥7 points | TR5 | Highly suspicious | ≥0.5 cm follow up, ≥1.0 cm FNAC | Annual follow up for up to 5 years | 35% |
FNAC is recommended for suspicious lesions (TR3 – TR5) with the above size criteria. If there are multiple nodules, two nodules with the highest ACR TI-RADS grades should be sampled (rather than the two largest).
Interval enlargement on follow up is felt to be significant if there is an increase of 20% and 2 mm in two dimensions, or a 50% increase in volume.
If the ACR TI-RADS level increases between scans, an interval scan the following year is again recommended.
Pros and Cons of ACR TI-RADS
Studies have shown that the ACR TI-RADS system has a sensitivity ranging from 75-97% and specificity ranging from 53-67%, resulting in lower rates of unnecessary fine needle aspiration (false positive rates).
Following are some of the limitations of the ACR TI-RADS system
- No category to indicate a normal thyroid gland, unlike other thyroid reporting systems, preserving ACR TI-RADS for lesion reporting.
- Thresholds for mildly suspicious and moderately suspicious nodules (2.5 and 1.5 cm, respectively) are higher than the cutoffs advocated by the ATA and the Korean Society of Thyroid Radiology. In a study by Machens et al, it was found that the cumulative risk for distant metastases from thyroid cancer increased once the primary tumor size was more than 2cm. They, therefore, recommended FNAC of nodules larger than 2 cm.
References
- Tessler FN, Middleton WD, Grant EG, Hoang JK, Berland LL, et al. ACR Thyroid Imaging, Reporting and Data System (TI-RADS): White Paper of the ACR TI-RADS Committee. (2017) Journal of the American College of Radiology : JACR. 14 (5): 587-595.
- Grant EG, Tessler FN, Hoang JK, Langer JE, Beland MD, Berland LL, Cronan JJ, Desser TS, Frates MC, Hamper UM, Middleton WD, Reading CC, Scoutt LM, Stavros AT, Teefey SA. Thyroid Ultrasound Reporting Lexicon: White Paper of the ACR Thyroid Imaging, Reporting and Data System (TIRADS) Committee. (2015) Journal of the American College of Radiology: JACR. 12 (12 Pt A): 1272-9.
- Hoang JK, Langer JE, Middleton WD, Wu CC, Hammers LW, Cronan JJ, Tessler FN, Grant EG, Berland LL. Managing incidental thyroid nodules detected on imaging: white paper of the ACR Incidental Thyroid Findings Committee. Journal of the American College of Radiology: JACR. 2015; 12 (2): 143-50.
- Ting Xu, Ya Wu, Run-Xin Wu, Yu-Zhi Zhang, Jing-Yu Gu, Xin-Hua Ye, Wei Tang, Shu-Hang Xu, Chao Liu, Xiao-Hong Wu. Validation and comparison of three newly-released Thyroid Imaging Reporting and Data Systems for cancer risk determination. (2019) Endocrine. 64 (2): 299.
- Floridi C, Cellina M, Buccimazza G, Arrichiello A, Sacrini A, Arrigoni F, Pompili G, Barile A, Carrafiello G. Ultrasound imaging classifications of thyroid nodules for malignancy risk stratification and clinical management: state of the art. Gland Surgery. 2019 Sep;8(Suppl 3):S233.