Tornwaldt cysts also spelled as Thornwaldt cyst or Thornwald cyst are benign, midline cystic swelling located in the roof of nasopharynx. It is also known as Pharyngeal bursa (Luschka Bursa).
The condition was first described by Gustav Ludwig Tornwaldt in the 1885 as one of the causes of pharyngeal discomfort. The original description of this cyst is thought to have been made by A F C J Meyer in 1840.
Epidemiology
The condition is relatively rare with a reported incidence of 1.4–3.3%, with no gender predilection in the literature. The disease usually presents between the age of 15–30.
The condition is usually asymptomatic and detected incidentally while evaluating for other clinical conditions.
Majority of cysts are undiagnosed due to their small size and benign nature. Some larger or infected cysts may cause symptoms like nasal obstruction, postnasal drip, headache, neck muscle stiffness, pharyngitis and Eustachian tube dysfunction. A symptomatic cyst is called as Tornwaldt disease.
Etiology
Obstruction of the pharyngeal bursa leads to formation of a Thornwaldt (or Tornwaldt) cyst. The bursa is located above the superior pharyngeal constrictor muscles, at about the level of the fossa of Rosenmuller. The bursa extends between the longus capitis muscles up to occipital tubercle (nasopharyngeal tubercle of the occiput). Obstruction of the nasopharyngeal orifice of the pharyngeal bursa leads to formation of the Thornwaldt cyst.
Trauma to nasopharynx due to conditions like nasopharyngitis, chemoradiation or adenoidectomy have also been implicated as the etiological factor in approximately 75% of cases.
Types
Based on the drainage Tornwaldt cysts are classified in to two categories, crusting and cystic. The cystic type has an obstructed drainage pathway resulting in a cyst formation, while the crusting type drains spontaneously into the nasopharynx.
The cyst is lined by respiratory epithelium and accumulates fluid with variable proteinaceous content, inflammation can occur due to obstruction.
Differential diagnosis
The differential diagnosis include normal/prominent adenoids, mucous retention cyst, minor salivary gland tumors, nasopharygeal carcinoma, neurenteric cysts and meningocoele.
Diagnosis
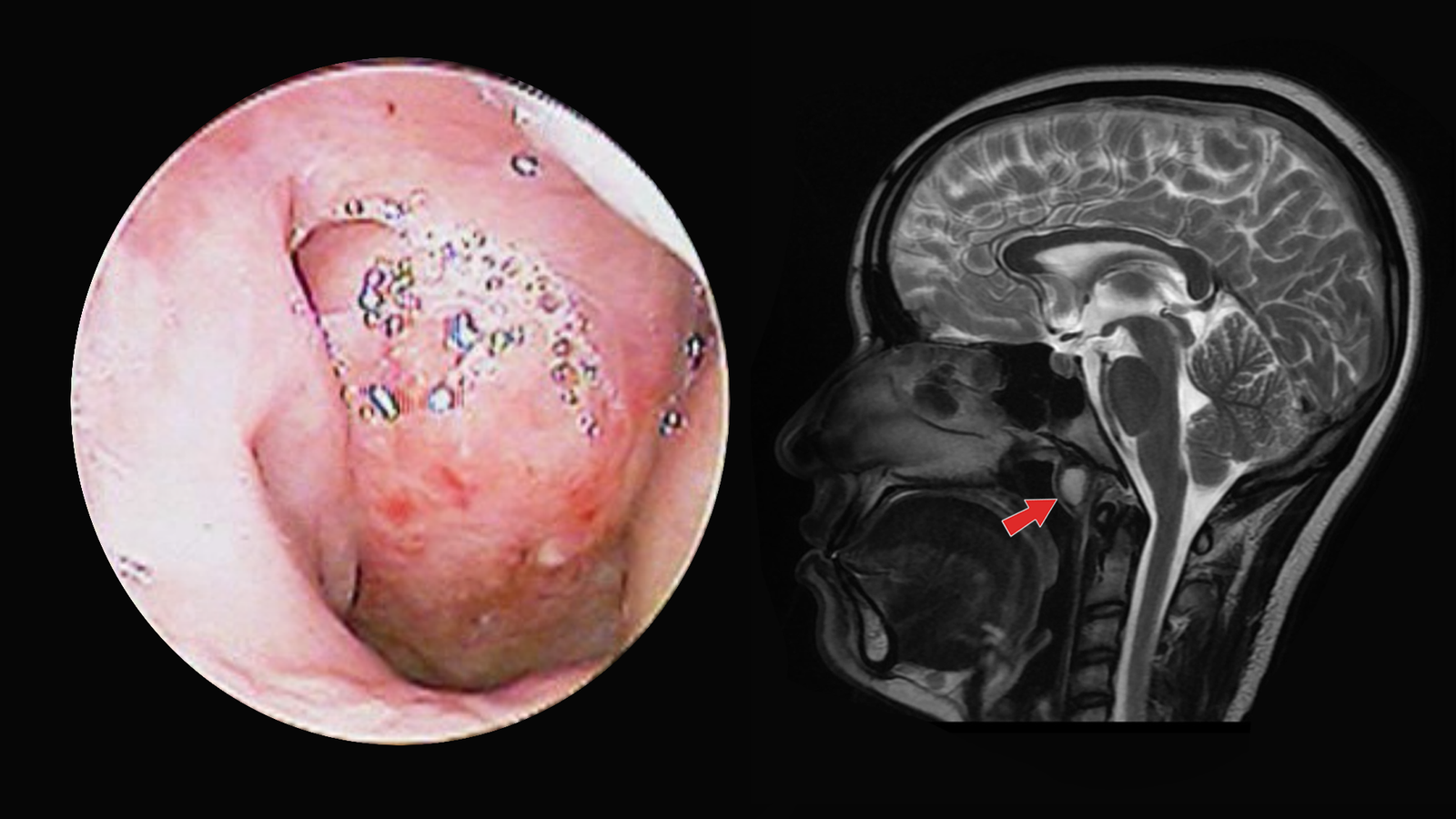
A simple diagnostic nasal endoscopy will reveal a smooth submucosal, well encapsulated mass along the roof of the nasopharynx. The mass is usually midline, but may be off-midline. The pharyngeal orifice of the bursa may be difficult or impossible to appreciate at clinical inspection, even when not obstructed.
If in doubt, imaging studies can confirm the diagnosis. MRI is the gold standard modality for detecting the cyst, evaluating its size, content and anatomical relationship to surrounding structures. Characteristic findings help to differentiate them from other sinister nasopharyngeal pathologies. MRI also helps to rule out any intracranial extensions.
In imaging they appear well circumscribed, thin walled rounded lesions immediately deep to the mucosa. They are variable in size, ranging from a few millimeters to a few centimeters in diameter, but are typically 2-10 mm in size. MRI demonstrates well circumscribed thin wall cysts with T2 high signal and no Gadolinium enhancement.
Treatment of Tornwaldt cyst
No intervention is required in asymptomatic cases. In symptomatic cases, surgical excision or marsupialization of the cyst, performed via a transnasal approach is enough. Thornwaldt cysts must be differentiated from nasopharyngeal encephaloceles before excision.
Surgical management can lead to complete resolution of symptoms in the vast majority of patients.