Acute tonsillitis is an inflammatory condition of tonsil lasting less than 3 weeks duration.
The tonsils are composed of lymphatic tissue and are a component of Waldeyer’s ring in the lateral oropharynx. They are found between the palatoglossal arch anteriorly and the palatopharyngeal arch posteriorly, known as the palatine arches or pillars. They serve as an important defense against ingested pathogens by providing the initial immunological barrier to insults
It may occur
- as an isolated episode
- in association with a viral upper respiratory tract infection (URTI) including generalized pharyngitis.
- most common viruses are rhinovirus, respiratory syncytial virus, adenovirus, and coronavirus.
- other viral causes such as Epstein-Barr (causing mononucleosis), cytomegalovirus, hepatitis A, rubella, and HIV may also cause tonsillitis.
- as a part of systemic infections like Infectious Mononucleosis (IMN)
- classically the causative organism is Group A β Hemolytic Streptococci (GABHS)
- Staphylococcus aureus, Streptococcus pneumoniae, and Haemophilus influenza have also been cultured.
- Corynebacterium diphtheriae causing diphtheria in unvaccinated patients.
- a wide variety of other organisms, anaerobes and virus are also implicated – HIV, syphilis, gonorrhea, chlamydia and Tuberculosis
Epidemiology
- It constitutes approximately 1.3% of outpatient visits
- The condition is more common in children, during autumn and winter months.
- GABHS accounts for 5% to 15% of adults with pharyngitis and 15% to 30% of patients between the ages of five and fifteen.
- GABHS is rare in children under two years of age.
- Viral etiologies are more common in patients under five.
Types of acute tonsillitis
- Acute catarrhal / superficial tonsillitis – Tonsillitis is part of generalized pharyngitis and mostly seen in viral infections.
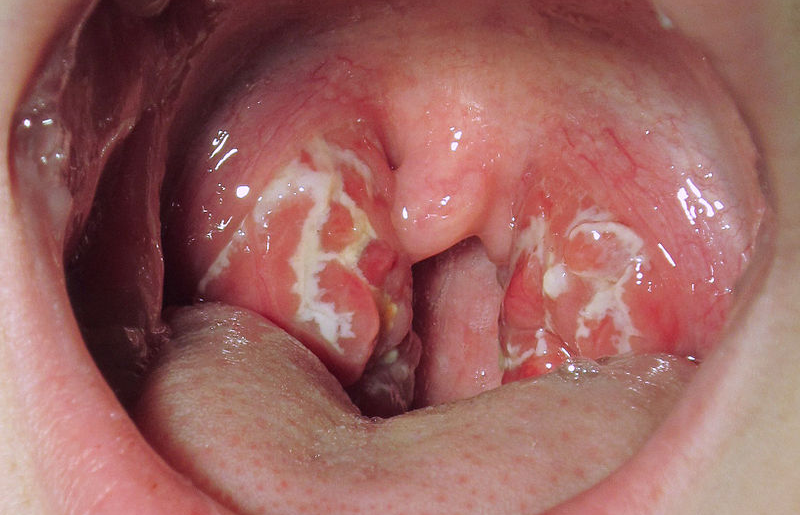
- Acute follicular tonsillitis – Infection spreads to tonsillar crypts which become filled with purulent material presenting at openings of crypts as yellow spots
- Acute membranous tonsillitis – Exudation from crypts coalesces to form a membrane on surface of tonsil.
- Acute parenchymatous tonsillitis – uniformly enlarged and red tonsil because of involvement of tonsil substance.
Clinical presentation
- Symptoms – History or fever, sore throat, painful swallowing
- Signs – pharyngeal congestion with or without tonsillar exudates, tender anterior cervical lymphadenopathy.
Differential diagnosis
- Pharyngitis, retropharyngeal abscess, epiglottitis, and Ludwig angina
- Dental or peritonsillar abscess
- Kawasaki disease, Coxsackie virus, primary HIV, Ebstein-Barr virus, and oral Candidiasis
Diagnosis
- Acute tonsillitis is a clinical diagnosis
- Microbiology
- Diagnosis of causative agent has little role in management as both bacterial and viral tonsillitis tend to resolve quickly without treatment in most cases. Hence throat swab and culture is usually indicated in severe cases only.
- Results can take upto 24-48 hours.
- Throat swab may yield positive culture for GABHS. But this may be false positive as positive culture is seen in upto 40% of asymptomatic carriers.
- Carrier states are common among false negative patients – can be identified by ASO titer assessment – will have a positive culture for hemolytic streptococci with a negative ASO titer.
- Rapid Antigen Test (RAT)
- This is an office procedure with high speed in reporting – results obtained usually within 10 minutes.
- Specific (88% to 100%) but is not sensitive (61% to 95%) – false negatives are possible.
- A mononucleosis spot test can be a consideration when the Ebstein-Barr virus is suspected (usually will have kissing tonsils).
- Imaging and other lab investigations are rarely necessary for uncomplicated infections.
- Indicated in patients with unstable vital signs, toxic appearance, inability to swallow, inability to tolerate oral intake, or trismus etc.
- CT imaging of the neck with intravenous contrast to exclude dangerous causes such as abscess, Lemierre disease, and epiglottitis.
- Complete blood count and basic metabolic panel to assess renal function, etc. also to be considered accordingly.
Treatment of acute tonsillitis
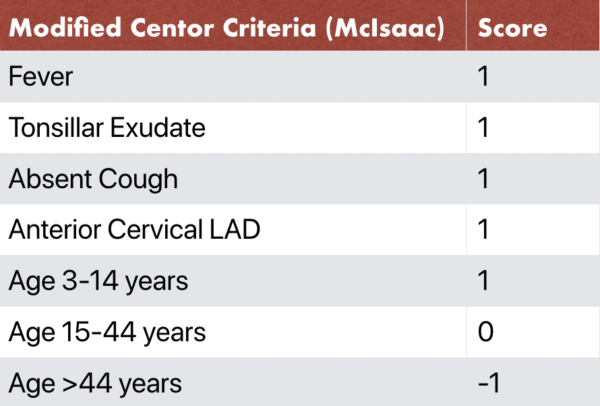
- Centor Scoring
- a four-point scoring system used to assist with risk stratification for pharyngitis and clinical decision making.
- The four components of the Centor Criteria are: fever, tonsillar exudate, anterior cervical lymphadenopathy, and absence of cough.
- The Centor Criteria was originally validated in patients 15 years of age and older. The McIsaac Criteria, which is also referred to as the modified Centor criteria, uses the same four clinical features, but also provides an age adjustment to the final score and can be used in patients 3 years of age and older.
- In patients scoring 0 to 1, no further testing or antibiotics is necessary. In patients scoring 2 to 3 points, rapid strep testing and throat culture is an option. In patients with scores of 4 or more, clinicians should consider testing and empiric antibiotics.
- For the majority of patients, tonsilitis is a self-limiting disease.
- Hospital admission is rarely necessary.
- Principally supportive with use of analgesics and adequate hydration.
- Paracetamol (Acetaminophen) is the first line.
- Specific treatment
- Average duration of an acute tonsillitis is 2-3 days.
- Antibiotics can shorten the duration of illness and can reduce the risk of sequel.
- But studies have shown only marginal evidence in blanket antibiotic therapy. Evidence shows only a limited role for antibiotics.
- Antibiotic therapy is recommended for patients.
- at high risk of bacterial pharyngitis based on Centor criteria and antigen testing or throat culture, antibiotics are often used in treatment.
- in whom no signs of improvement within 48-72 hours.
- with high rates of complications, especially rheumatic heart disease and rheumatic fever.
- Drug of choice is penicillins for a seven-ten-day oral regimen course / or a single benzathine penicillin G intramuscular injection.
- In patients who are allergic to penicillins a 5-day course of azithromycin or a 10-day course of cephalosporin to be considered.
- A single dose of dexamethasone as adjuvant therapy is of significant benefit in reducing pain of acute tonsillopharyngitis with no evidence of predisposition to abscess formation.
Prognosis
- Most cases are self-limiting infections with excellent prognosis.
- In cases with GABHS complications, (e.g. rheumatic fever and glomerulonephritis) patients can have long-term sequela, like cardiac valvular disease and decreased renal function.
- Alternative diagnosis like HIV, Tuberculosis, gonorrhea, chlamydia, syphilis, mononucleosis, Kawasaki disease, abscess, and Lemierre syndrome should be suspected in patients with no symptomatic improvement.
Complications of acute tonsillitis
- Systemic complications
- Sepsis – septicemia, septic arthritis
- GABHS – exanthematous reaction – Scarlet fever, Rheumatic fever and Glomerulonephritis.
- Psoriasis exacerbation – mainly by GABHS – probably immune related
- Local complications
- Peritonsillar cellulitis
- Peritonsillar abscess / Quinsy
- Retropharyngeal Abscess (RPA)
- Parapharyngeal Abscess (PPA)
- Lemierre’s syndrome
- Recurrent tonsillitis
- Recurring infections every few weeks or months arbitrarily defined as five or more tonsillitis episodes in one year.
- There is currently no way in predicting those individuals whom recurrence can happen.
- Primary immunodeficiency requires consideration in such patients.
- Supportive measures continue to be appropriate, and management of more severe symptoms may need antibiotic therapy.
- Tonsillectomy should be recommended in cases where quality of life is affected (refer Paradise criteria for tonsillectomy).
- Subacute tonsillitis
- Clinical condition where patient is never free from discomfort in throat associated with enlarged inflamed looking tonsil punctuated with acute episodes which may be either mild or severe.
- Chronic tonsillitis
- Chronic low grade symptoms like feeling of ill health, throat discomfort, production of unpleasant smelly white or yellow debris from tonsillar crypts lasting more than 3 weeks.
- Squeeze test / Irwin Moore sign – squeezing out of pus / whitish material from the tonsillar follicles on pressing of anterior pillars is a classical sign in chronic tonsillitis.
- Children with chronic tonsillitis may have failure to thrive, low body weight etc. Recommend tonsillectomy in such cases.
- Rarely these debris may become inspissated and calcified to form tonsillolith.
- Types of Chronic tonsillitis
- Chronic Follicular tonsillitis: Tonsillar enlargement is associated with the presence of prominent inflamed follicles.
- Chronic parenchymatous tonsillitis: Tonsils are enlarged but the follicles are not prominent. Infection is found within the substance of the tonsil.
- Chronic fibroid tonsils: Tonsils are small, infected with repeated history of sore throats.