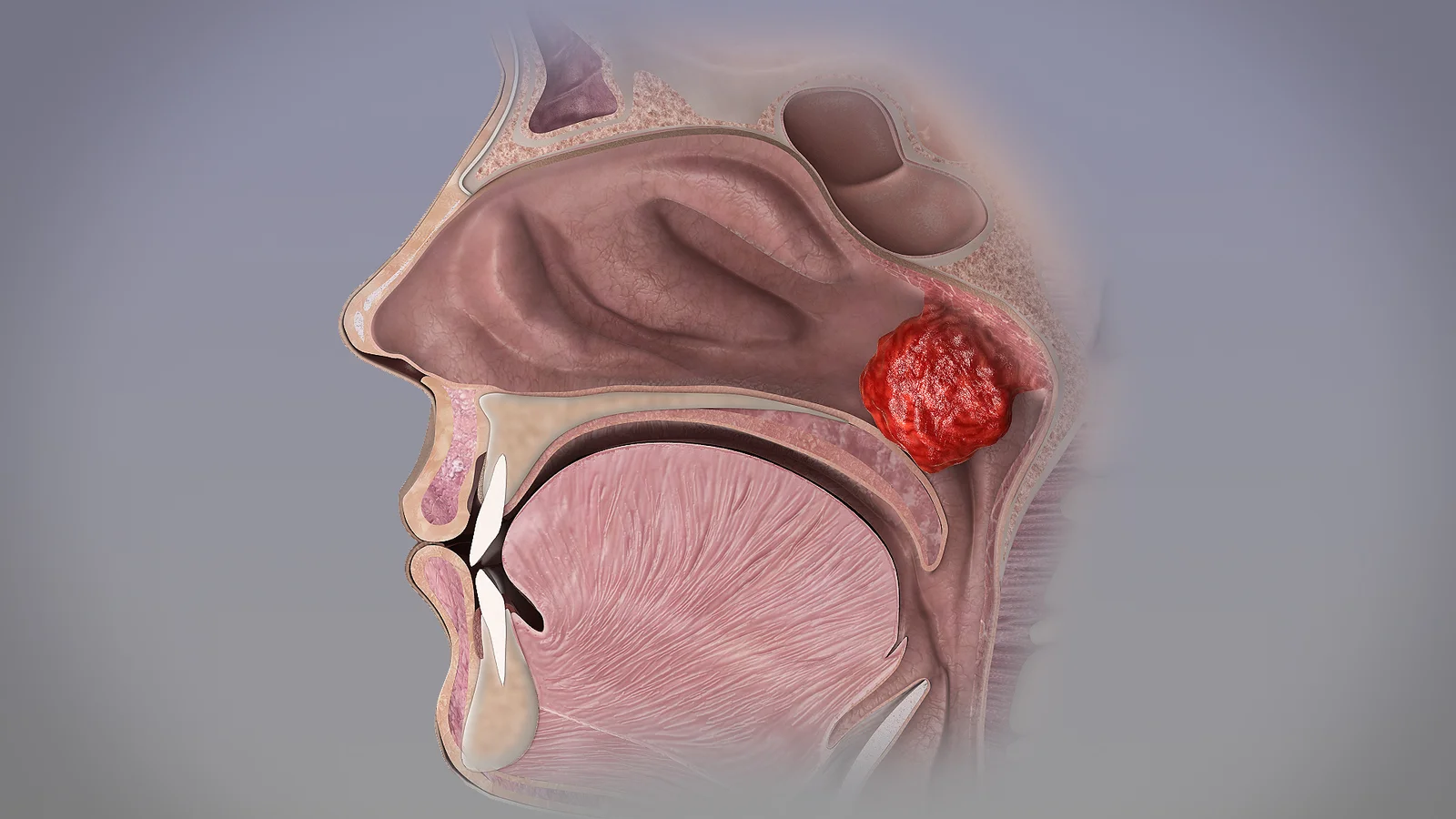
Adenoids are a subepithelial collection of lymphoid tissue, which is present at the junction of the roof and posterior wall of the nasopharynx. They increase in size up to the age of 6 years and after that gradually atrophies.
- Adenoids are part of Waldeyer’s ring of lymphoid tissue at entry of upper respiratory tract. These are sites of first immunological contact for inhaled antigen in childhood.
- The word adenoid was coined by Wilhelm Meyer. They are also known as Lushka’s tonsil (by Santorini), Nasopharyngeal vegetations/ and nasopharyngeal tonsils.
Anatomy
- Adenoids consists of vertical ridges of lymphoid tissues separated by deep clefts and covered by ciliated epithelium.
- Unlike palatine tonsils, adenoids have no crypts or capsules.
Development
- By around 4-6 weeks of gestational age, lymphoid tissues can be identified with in mucus membrane of roof and posterior wall of nasopharynx.
- These lymphoid tissues may extend to fossa of Rossenmuller and to eustachian tube orifice (Tubal tonsils / Gerlach’s tonsil)
- Adenoids can be identified by MRI from 4th month in 18% children and by 5th month in all children.
- Growth continues rapidly during infancy and plateaus between 2-14 years.
- Largest in 7th year, but clinical symptoms are more common in young age group due to
- Relatively small volume of nasopharynx
- Increased frequency of Upper respiratory tract infections
- Regression occurs rapidly after 15 years and completely disappears by 20 years.
Blood supply and Venous drainage
- Blood supply via
- Ascending palatine branch of facial artery
- Ascending pharyngeal branch of External Carotid Artery (ECA)
- Pharyngeal branch of third part of maxillary artery
- Ascending cervical branch of inferior thyroid artery of thyrocervical trunk
- Venous drainage to IJV and Facial vein.
- Lymphatic drainage to retropharyngeal LN, upper deep cervical LN (post triangle)
- Nerve supply – Sensory branches of vagus and glossopharyngeal.
Functions of adenoid
- Produce B cells, producing IgG, IgA Ab.
- Forms immunologic memory in younger children.
Pathological effects
- Can act as a focus of sepsis / infection.
- Recurrent Otitis Media with Effusion (OME)
- Due to anatomical obstruction of eustachian tube along with recurrent Acute or chronic inflammation of adenoid and increased bacterial load (particularly H. influenza).
- Biofilm formation
- Biofilms are structured bacterial cells enclosed in a self-produced polymeric matric, adherent to an inert of living surface)
- Causes squamous cell metaplasia – reticular epithelium extension – fibrosis of interfollicular connective tissues – reduced mucociliary clearance – biofilm formation.
- Chronic GERD is also implicated in inflammation of nasopharynx and adenoids leading to recurrent OME.
- Recurrent Acute Otitis Media (AOM)
- Evidence says that adenoidectomy is not effective in reducing episode of AOM in children <2 years.
- Low dose prophylactic antibiotics, until maturation of immune system is preferred to adenoidectomy in these children to prevent recurrence.
- Upper airway obstruction
- Nasal obstruction is the most common symptom.
- Mouth breathing interferes with feeding or suckling in child leads to failure to thrive.
- Obstructive Sleep Apnea (OSA)
- Incidence of OSA in children is approximately 1% with equal sex ratio.
- Peak incidence at 3-6 years.
- Airway obstruction by adenoid causes – decreased PaO2, Increased PaCO2, and decreased IGF-1. All returns to normal after adenoidectomy.
- Radiographic findings of adenoids correlate well with PSG findings.
- Rhinitis
- Due to choanal obstruction, normal nasal secretions cannot drain into nasopharynx.
- Chronic rhinosinusitis
- Improvement noted in majority of children following adenoidectomy.
- Due to biofilm formation
- Olfaction
- Olfactory sensitivity is reduced in relation to adenoid size and improves after adenoidectomy.
- May be leads to poor appetite in children with adenoid hypertrophy.
- Nocturnal enuresis
- Significant relief after adenoidectomy.
- Adenotonsillectomy can improve bedwetting in kids – Read article.
- Upper airway obstruction causes deep inspiration, leads to increased venous return to mediastinum. This will cause dilatation of atrial muscles, which in turn cause release of ANP/BNP. As a result, diuresis happens.
- Pulmonary hypertension
- In long standing nasal obstruction.
- Neoplasia
- Unsuspected neoplasia of adenoid and tonsil in childhood is rare.
- Atypical lymphadenopathy, persistent and asymmetric enlargement of adeno-tonsills in absence of infection are suspicious of malignant transformation – needs early imaging and biopsy.
- Diagnosis is mainly overlooked for infections.
Assessment and Management
- Clinical history
- Full pediatric ENT history
- Special attention to symptoms of middle ear disease, nasal obstruction.
- Specific questions regarding sleep disturbances, eating and atopic symptoms.
- Aprosexia – loss of concentration.
- Full history of previous treatment and medications.
- Family history of unusual bleeding / bleeding tendency, if planning for surgery.
- Examination
- Adenoid facies
- Due to chronic nasal obstruction and mouth breathing.
- Elongated face with dull expression, dark circles under eyes.
- Open mouth, Retrognathic mandible, hitched up upper lip, prominent and crowded upper teeth, pinched up nose (due to disuse atrophy of alae nasi).
- High arched / Gothic palate due to loss of molding action of tongue on palates.
- External nose – skin crease in supratip region indication frequent rubbing due to rhinitis.
- Anterior rhinoscopy – Cold spatula test, using Lack’s tongue depressor to assess airway patency.
- Diagnostic Nasal Endoscopy with topical intranasal anesthetic spray is the gold standard.
- Well tolerated in children
- For treatment decision prior to adenoidectomy
- Endoscopic grading system co-relates well with symptoms of nasal obstruction, snoring, tympanometry. But no co-relation with purulent rhinorrhea.
- Adenoid facies
- Imaging
-
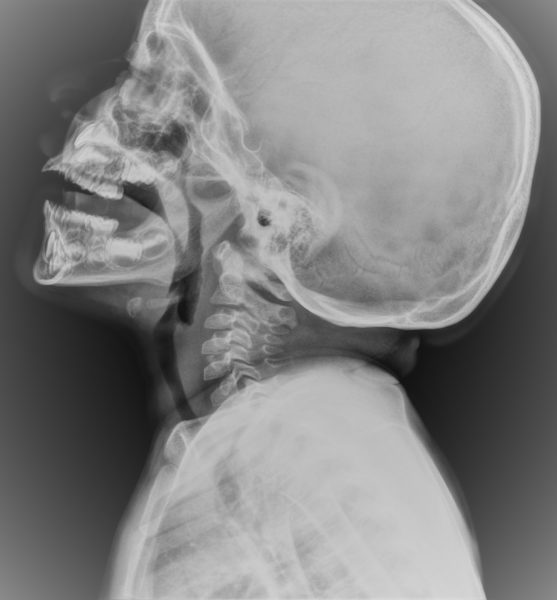
Xray Neck Lateral View Showing Adenoid Hypertrophy Soft tissue Xray neck Lateral View is also a good alternative to nasal endoscopy, indicated if child is not co-operative for nasal endoscopy.
(Click here to read doctor’s own study on this subject.) - Clemens et al radiographic grading
- Grade I – Adenoid tissue filling 1/3rd of vertical portion of choanae.
- Grade II – Adenoid tissue filling 1/3rd to 2/3rd of vertical portion of choanae.
- Grade III – Adenoid tissue filling 2/3rds to nearly complete obstruction of choanae.
- Grade IV – Complete choanal obstruction
- Acoustic rhinomanometry and MRI are not applicable in clinical practice.
-
Adenoidectomy
- Surgical procedure for removing of enlarged adenoids (Adenoid Hypertrophy).
- Unless specifically indicated, combining tonsillectomy with adenoidectomy is not recommended. This is because compared to adenoidectomy, tonsillectomy is associated with a significantly increased mortality of 1:10,000 to 1:35,000, increased complication rates, treatment costs and with a post op bleeding rate of 0.6% to 4%, occurring in the immediate perioperative period and up to two weeks postoperatively.
- Indications
- Symptomatic patients.
- Generally, if >45% obstruction of airway is there (Grade 2 adenoids), it is considered as an indication.
- Impact of adeno-tonsillectomy
- Adenoid hyperplasia in childhood is common and self-limiting usually.
- Removal at young age (< 3 years) may be immunologically undesirable, unless highly indicated.
- Between 4-10 year, adeno-tonsillectomy doesn’t cause immune deficiency.
- Procedure
- Under General Anesthesia with child in tonsillectomy position (Rose’s position).
- Traditionally
- Assessment of adenoids done by digital palpation and soft palate for any submucosal cleft.
- Removal is by blind curettage with St. Clair Thomson’s curette with guard – chance of left over tissue, leading to recurrence.
- Hemostasis achieved by gauze swab tamponade.
- More blood loss (>50ml)
- Other options
- Under Endoscopic Visualization
- Less blood loss (<4ml)
- Near total removal – very minimal chance of recurrence.
- Avoiding trauma to eustachian tube
- Microdebrider – 20% faster
- Suction coagulator – significantly cheaper than debrider
- Coblation assisted – costly, but less painful.
- KTP laser – High incidence of post op nasopharyngeal stenosis – not recommended.
- Under Endoscopic Visualization
- Complications
- Dental trauma
- Usually rare.
- May be accidental due to slippage of gag or support.
- When loose dentition present, needs to be removed prior to surgery.
- Parents should be warned about damage to teeth.
- Bleeding
- Primary / Reactionary hemorrhage (within 6-24 hours) is less than 0.7%
- If severe, Posterior nasal packing for 4 hours has shown same efficacy as 24hours. Immediate return to theatre also needed.
- Less chance following endoscopic resection.
- Usually due to bleeding from aberrant ascending pharyngeal artery
- Secondary hemorrhage (after 24 hours) is rare.
- Clotting disorders – Needs hematological advice.
- Retained swab.
- Count should be made before removal of gag and reversal of anesthesia.
- Swab may be retained in nasopharynx or laryngopharynx.
- Nasopharyngeal blood clot
- Gentle suction before removal of gag.
- If not done, clot will fall to larynx during extubating causing fatal acute airway obstruction – Coroner’s Clot.
- Infections
- Uncommon.
- Fetor (bad breath) may be common for a week.
- Rarely retropharyngeal and mediastinal abscess ay occur due to trauma and secondary infection of adenoid bed.
- Cervical spine injury
- Griesel syndrome – non-traumatic atlanto axial subluxation is rare.
- Mostly due to spasm of paraspinal muscles – associated with overuse of diathermy – minimum power settings are recommended.
- More prone in patients with Down syndrome – due to laxity of ligaments. Prior plain imaging of cervical spine needed.
- Patient present with torticollis, neck pain.
- Velopharyngeal dysfunction
- Severe dysfunction seen in 1:1500-10,000 cases.
- Velopharyngeal Insufficiency
- Hypo nasal speech, swallowing, nasal regurgitation of food.
- Prior to surgery, palate and uvula needs to assess for submucosal cleft, palatal dysfunction.
- In children with bifid uvula or with submucosal cleft, partial removal under endoscopic guidance with clearing of choanal airway but leaving adenoid intact at velopharyngeal junction is done by some – controversial.
- Long term velopharyngeal insufficiency is rare, reconstructive surgery to correct hyper nasal speech and swallowing.
- Other complications
- Injury to eustachian tube
- Injury to pharyngeal musculature and vertebrae
- Regrowth
- If needed, repeat surgery can be done.
- More in traditional blind curettage
- Dental trauma
- Post op care
- Mostly day care procedure
- Based on social & geographic factors, surgical & anesthetic techniques, fluid replacement, Antibiotics & analgesia – child can be discharged within 6 hours.