Malignant otitis externa (MOE) is an aggressive and potentially life-threatening infection of the soft tissues of the external ear and its surrounding structures, which quickly spreads to involve periosteum and bone of the skull base.
The most common causative organism of malignant otitis externa is Pseudomonas aeruginosa.
Though this is not a neoplastic disease, it’s named so because of the high morbidity associated. The disease is also known as skull base osteomyelitis or necrotizing otitis externa.
Meltzer, in 1959 reported the first case of pseudomonas osteomyelitis of temporal bone. Chandler in 1968, discussed the various clinical features and described it as a distinct clinical entity.
Pathology of Malignant Otitis Externa
Malignant otitis externa is an end-stage of severe infection that originates from the external auditory canal of the ear and progresses through stages of cellulitis, chondritis, periostitis, osteitis and finally osteomyelitis.
The disease mainly affects the Haversian system of compact bone. Hence the involvement of pneumatized part of the temporal bone is a late finding.
Once periostitis develops, the infection spreads rapidly across the skull base via the Haversian system causing cranial nerve palsies.
Predisposing factors
Malignant otitis externa is most commonly found in immunocompromised (eg: AIDS, cancer) patients. Other predisposing factors are diabetes mellitus, renal cell carcinoma, etc.
The disease is more commonly observed in elderly diabetics. Various theories are proposed supporting the association of diabetes and MOE. These include the impaired host response, microangiopathy in diabetic tissues exacerbated by vasculitic properties of pseudomonas, altered (higher) pH of cerumen (ear wax) in diabetic patients than normal controls with the reduced bactericidal property.
One-third of cases are non-diabetic and the infective organism in these patients is found to be usually non-pseudomonas. The reported species in such cases include Aspergillus, Staphylococcus aureus, Proteus mirabilis, Klebsiella oxytoca, Burkholderia cepacia and Candida parapsilosis, etc.
Recent ear surgery and irritation caused be hearing aids may also be risk factors for malignant otitis externa.
Unlike elderly adults, MOE in children is very rare, with less than 20 cases reported in the literature. These children are more likely to be immuno-compromised (eg, malignancy or malnutrition).
Diagnosis of Malignant Otitis Externa
Diagnosis of MOE is mostly on clinical features like ear discharge, continuous ear pain worsening in the night, resistance to local therapy (for 8-10days), granulation tissue and edema of the external auditory canal.
The presence of granulation tissue in the floor of the external auditory canal, at the bony cartilaginous junction (at the site of Santorini’s fissures), is a cardinal sign of skull base osteomyelitis.
Levenson’s criteria for the diagnosis of malignant otitis externa include.
- Refractory otitis externa
- Severe nocturnal otalgia, out of proportion to clinical symptoms
- Purulent otorrhea
- Granulation tissue in the external ear canal
- Growth of Pseudomonas aeruginosa from the external ear canal
- Presence of diabetes and other immunocompromised states
The facial nerve is the earliest cranial nerve to get affected. Once the disease starts progressing, followed by other higher cranial nerves (IX, X, XI, XII) also get affected. Cranial nerve V and VI and rarely affected at the petrous apex.
Facial palsy occurs early in children due to their relatively undeveloped mastoid process and the more medial location of the fissures of Santorini, which places the facial nerve in closer proximity to the ear canal.
Because of significant differences in natural course and treatment, it is crucial to differentiate severe otitis externa and necrotizing external otitis. The involvement of structures beyond the soft tissues of the auditory canal occurs only in necrotizing otitis externa.
A positive bone scan, the presence of micro-abscess at the surgery is confirmatory for diagnosis of MOE.
Investigations
Erythrocyte Sedimentation Rate (ESR) and C-Reactive Protein (CRP), though non-specific to MOE, are found to be raised. ESR may increase above 100mm/hour. ESR and CRP rates are also used to assess the response to treatment.
Bacterial and fungal culture along with antibiotic sensitivity should be done when ear discharge is present. If signs of systemic toxicity (eg, fever) are present, blood cultures should be obtained.
Biopsy from the granulation tissues should be obtained which helps in differentiating a tumor from necrotizing infection.
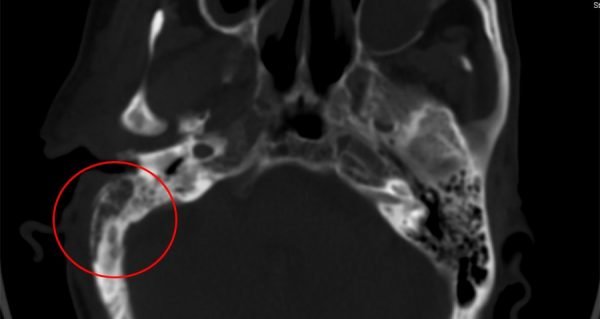
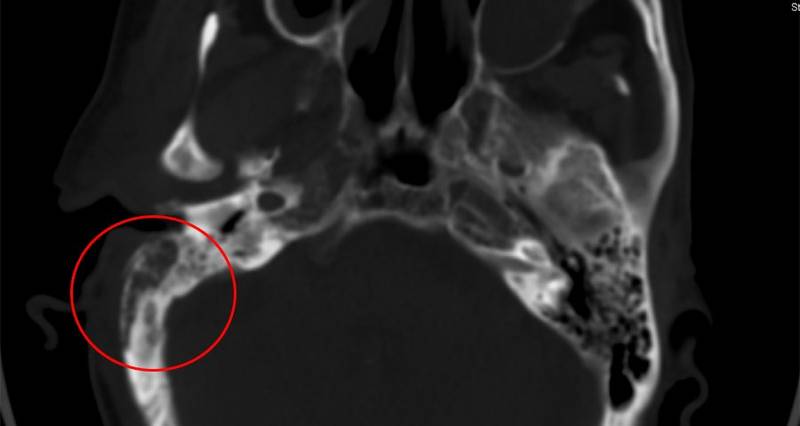
High resolution computed tomography (HRCT) imaging of temporal bone helps in both anatomic localization of disease as well as the assessment of disease resolution. HRCT is ideal for assessment of bone erosion. Demineralization of bones is the characteristic finding.
MRI (Magnetic Resonance Imaging) will show increased signal intensity in soft tissues beneath the skull base due to inflammation. MRI is also helpful to know the extent of disease, to differentiate between a malignant and inflammatory process too.
Technetium 99 (Tc99) scan can detect bone involvement even before HRCT detects. The isotope is absorbed by both the osteoclasts and osteoblasts, which continues remodeling even after infection settles. This may make the scan positive for up to 9 months. Hence Technetium 99 scan is useful only for initial bone involvement.
Gallium citrate (Ga 67) and Indium 111 are two other isotopes which are absorbed by leukocytes and bacteria and is a more sensitive indicator of infection. Ga 67 is taken up by any inflammatory process including simple otitis externa – useful for monitoring than a diagnosis. It returns to normal after the infection subsides which helps in determining when to stop treatment.
SPECT-CT (Single-photon emission computed tomography) helps in spatial localization of the disease extent and anatomy. But this is expensive and has limited availability only.
Staging of Malignant otitis externa
Malignant otitis externa is staged into 4:
| Stage 1 | Clinical evidence of malignant otitis externa with infection of soft tissues beyond the external auditory canal, with a negative Tc99 bone scan. |
| Stage 2 | Soft tissue infection beyond the external auditory canal, but with positive Tc99 bone scan. |
| Stage 3 | Stage 2 + Cranial nerve palsy 3a: Single nerve palsy 3b: Multiple nerve palsy |
| Stage 4 | Meningitis, Empyema, Sinus thrombus or brain abscess. |
Management of Skull base osteomyelitis
Diagnosis of MOE needs a high index of suspicion, in an elderly diabetic patient with an earache and ear discharge.
Once the diagnosis of MOE is made, the management should be aggressive and should extend for long periods as this is a fatal disease.
Regular aural toilet is essential to control granulation and for pain control.
The role of topical antibiotics is controversial.
The treatment of choice for malignant otitis externa is culture-specific systemic antibiotics.
Because of poor vascularization of the target area, high-dose antibiotic therapy is needed to treat malignant otitis externa. Treatment should be continued for at least 6 weeks and in advanced cases for several months.
Following intravenous antibiotics are the most commonly used ones in the initial treatment period.
- Quinolones – Ciprofloxacillin, 400 mg intravenously every 8 hours; 750 mg orally every 12 hours is the drug of choice.
- Antipseudomonal beta-lactam agents – Carbenicillin, Piperacillin, Piperacillin-Tazobactam, Ticarcillin can be used.
- Third and fourth generation cephalosporins – ceftazidime, cefepime can also be used.
- Gentamycin can also be administered parenterally in doses of 80 mg iv two times a day in adults.
- Oral Rifampicin, Tobramycin, Implantable gentamicin beads (ototoxicity is a side effect) are used with some success.
| Summary of antibiotics used in the treatment of Malignant Otitis Externa | ||
| Antibiotic | Adult dosage | Dosage in children |
| Ciprofloxacin* | 400 mg intravenously [IV] every 8 hours.
750 mg orally every 12 hours |
20 to 30 mg/kg per day IV divided every 12 hours, not to exceed 800 mg/day.
20 to 30 mg/kg per day orally divided every 12 hours, not to exceed 1500 mg/day. |
| Piperacillin | 3 g IV every four hours or 4 g IV every six hours; | 50 to 75 mg/kg IV every four to six hours (not to exceed 4 g per dose or 24 g per day). |
| Piperacillin-Tazobactam | 4.5 g IV every six hours; in children ≤40 kg, 300 mg/kg of the piperacillin component per day IV divided every eight hours (not to exceed 16 grams per day of the piperacillin component); | in children >40 kg, 3 grams every six hours or 4 grams every six to eight hours. |
| Ceftazidime | 2 g IV every eight hours; | 100 to 150 mg/kg per day IV divided every eight hours (not to exceed 6 g per day). |
| Cefepime | 2 g IV every 12 hours is the standard dose (some clinicians use 2 g IV every 8 hours for severe P. aeruginosa infections); | 50 mg/kg IV every eight hours (not to exceed 2 g per dose). |
| *Use in children < 18 years should be with caution. | ||
Once CRP / ESR levels start falling, intravenous antibiotics can be stopped and can be changed over to oral antibiotics. The duration of therapy must be individualized on the basis of the clinical presentation (night pain, physical findings), ESR, and imaging studies.
Antifungals are useful when fungal growths are observed in the culture. The most commonly used antifungals are Voriconazole, Amphotericin B and Itraconazole. Of this Voriconazole is considered as the first line of treatment and should be given for more than 12 weeks. Liposomal Amphotericin helps in avoiding nephrotoxicity of Amphotericin.
Surgery in malignant otitis externa no longer has the goal of removing all infected tissues and should be reserved for a few selected cases. Surgery for removal of sequestrum, collection of pus, debridement of necrotic and granulation tissues can be beneficial but indicated only if the patient is deteriorating.
Vigilant management of the underlying immuno-compromised condition like diabetes is one of the most crucial steps in the treatment of malignant otitis externa.
There are some recent studies on the role of hyperbaric oxygen in the treatment of malignant otitis externa, with which some claim good results. But a randomized control trial is still needed to establish its role and at present, there is no clear evidence to demonstrate the efficacy of hyperbaric oxygen treatment over antibiotics.
In cases that are refractory to above line of management, other conditions like histiocytosis, malignancy of temporal bone, etc. need to be ruled out. Biopsy of the granulation, and other causes of immuno-compromise like AIDS, etc. needs to be evaluated for.
Complications
Anteriorly the infection spreads along the fissures of Santorini (congenital defects in the floor of the external auditory canal) to involve the temporomandibular joint, parapharyngeal space, etc. The involvement of temporomandibular joint results in trismus and pain while chewing.
Posteriorly disease spread involves mastoid and sigmoid sinus.
Medially disease progression can cause extensive skull base osteomyelitis eroding the clivus and even contralateral temporal bone may be involved. The infection then may extend into sphenoid and to the carotid. The otic capsule is usually spared.
Skull base osteomyelitis can cause progressive cranial nerve palsies. The facial nerve is the most commonly affected cranial nerve (60%) followed by IX, X, XI nerves. Cranial nerve VI and XII rarely involved.
Intracranially, the disease can spread to central venous sinuses, extradural spaces, meninges. Infective thrombophlebitis, thrombosis of the internal carotid artery, etc. are terminal events.
Treatment outcomes
These days, because of the early diagnosis and aggressive management mortality due to MOE is reduced to less than 10%. Prognosis is adversely affected by comorbid conditions, which are common in patients who develop malignant otitis externa.
The presence of cranial nerve palsy is a sign of advanced disease and can have a high mortality rate (up to 80%).
If successfully treated facial palsy may resolve completely in 22% cases and partially in 9%.
Prevention
In most patients with MOE, the initiating event may be self-inflicted or iatrogenic trauma to the ear canal.
Susceptible patients should be instructed to avoid manipulation of the external auditory canal (i.e., they should avoid self-cleansing of ear canals even with soft cotton buds). Cleaning of the external auditory canal, including aural irrigation by medical staff, should be carried out with extreme caution to avoid injuring delicate skin in the canal.
If these patients have any underlying eczematous conditions causing pruritis of the ear canal, it should be treated topically.
References
- Rubin Grandis J, Branstetter BF 4th, Yu VL. The changing face of malignant (necrotizing) external otitis: clinical, radiological, and anatomic correlations. Lancet Infect Dis 2004; 4:34.
- Bernstein JM, Holland NJ, Porter GC, Maw AR. Resistance of Pseudomonas to ciprofloxacin: implications for the treatment of malignant otitis externa. J Laryngol Otol 2007; 121:118.
- Chandler JR. Malignant external otitis. Laryngoscope. 1968;78:1257–94.
- Salit IE, Miller B, Wigmore M, Smith JA. Bacterial flora of the external canal in diabetics and non-diabetics. Laryngoscope 1982; 92:672.
- Joshua BZ, Sulkes J, Raveh E, et al. Predicting outcome of malignant external otitis. Otol Neurotol 2008; 29:339.
- Stevens SM, Lambert PR, Baker AB, Meyer TA. Malignant Otitis Externa: A Novel Stratification Protocol for Predicting Treatment Outcomes. Otol Neurotol 2015; 36:1492.Sadé J, Lang R,
- Goshen S, Kitzes-Cohen R. Ciprofloxacin treatment of malignant external otitis. Am J Med 1989; 87:138S.
- Levenson MJ, Parisier SC, Dolitsky J, Bindra G. Ciprofloxacin: drug of choice in the treatment of malignant external otitis (MEO). Laryngoscope 1991; 101:821.
- Phillips JS, Jones SE. Hyperbaric oxygen as an adjuvant treatment for malignant otitis externa. Cochrane Database Syst Rev 2013; :CD004617.