Acute Otitis Media (AOM) is a clinical condition defined as sudden onset inflammation of mucosal lining of middle ear and mastoid air cells by pyogenic organisms for less than 6 weeks duration.
Risk factors
- Age – Highest incidence of AOM is between 6 and 11 months of age and onset of AOM before 12 months of age is a powerful predictor for recurrence.
- Allergy – Role of allergy as etiology of acute otitis media is controversial.
- Immuno-comprised status – clinical conditions like agammaglobulinemia should be suspected in kids with recurrent AOM, especially bilateral cases.
- URTI – Recurrent attacks of common cold, upper respiratory tract infections, Fever (measles), Tonsils, adenoid infection, Chronic rhinitis and sinusitis
- Tumors of nasopharynx
- Nasal packing, Cleft palate, Use of pacifier, Low socio-economic status, Passive smoking
- Genetic
- Growing evidence that recurrent AOM is largely genetically determined.
- Relative risk of AOM in family members is 2.63
- Certain HLA types are associated with increased risk of Acute Otitis Media
- Maternal blood group A is an independent risk factor – Relative risk 2.82
Types of Acute Otitis Media
- Sporadic – Episodes of Acute Otitis Media occurring as infrequent isolated events, typically associated with URTI.
- Resistant – Persistent of symptoms and signs of middle ear infection beyond 3 to 5 days of antibiotic therapy.
- Persistent – Persistence or recurrence of symptoms and signs within 6 days of finishing a course of antibiotic therapy.
- Recurrent – Either 3 or more episodes of Acute Otitis Media occurring within a 6-month period of at least 4 or 6 episodes within 12-month period.
Routes of infection
- Ascending infection via eustachian tube
- In infants eustachian tube is short, wide and horizontal; hence is more prone for aspiration of milk and feeds into the middle ear cavity.
- Swimming and diving
- Spread of infection from external ear – In case of traumatic, perforations of tympanic membrane
- Blood born – this route is uncommon.
Causative organisms
- Most common pathogen is viral.
- Viral – Respiratory Syncytial Virus (RSV) > Influenza A > Adeno virus > Para influenza
- Bacteriology – H. Influenza (26%) > Moraxella (21%) > Strep. Pneumonia (3%) > Staph. Aures. 26% no growth isolated
- Fungal – Aspergillus, Candida
Pathology & Clinical features
- Rapid onset of otalgia (earache), hearing loss, otorrhea (ear discharge), fever, excessive crying, irritability, coryzal symptoms, vomiting, poor feeding, ear-pulling and clumsiness.
- AOM most commonly develops 3 to 4 days after onset of coryzal symptoms.
- Otalgia will settle in 60% of children without any treatment.
Stages of Acute Otitis Media
- Stage of tubal occlusion
- Edema, Hyperemia of nasopharyngeal end of eustachian tube leads to tubal blockage – this causes absorption of air in middle ear creating negative intratympanic pressure – causes some degree of middle ear effusion.
- Symptoms – Deafness (>20dB), earache, No fever
- Signs – Retracted tympanic membrane, in case of effusion membrane may appear bulging.
- Audiology – Conductive hearing loss
- Stage of pre suppuration
- Invasion of Tympanic cavity by pyogenic organisms / Antigen – Hyperemia, Exudation and congestion of tympanic membrane
- Symptoms – Marked earache, Throbbing nature, and sleep disturbance.
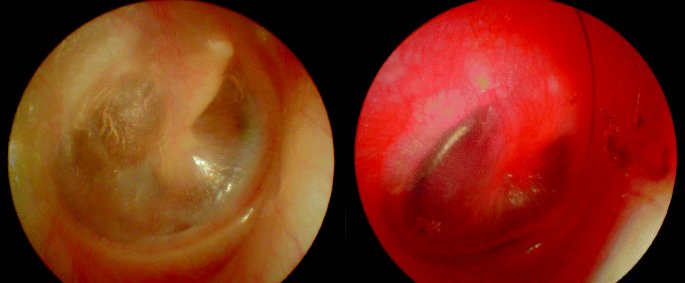
- Signs – Hyperemia, Exudation, Congestion of tympanic membrane, Cartwheel appearance of the membrane
- Audiology – Conductive hearing loss
- Stage of suppuration
- When early inflammatory stages fail to eradicate the disease.
- Recruitment of immune factors like CK, IL2, IL6, TNF alpha, Platelet endothelial cell adhesion molecule – Leaking blood vessels – Formation of pus in middle ear, mastoid air cells.
- Symptoms – Excruciating earache, increase deafness, High fever.
- Signs – Red bulging tympanic membrane, yellow spots, Tenderness over mastoid antrum.
- Audiology – Conductive hearing loss
- Xray mastoid – Clouding of air cells.
- Stage of resolution
- Varies in time.
- Fluid can remain in ear due to edematous eustachian tube and can cause otitis media with effusion.
- Rupture of tympanic membrane with release of pus, subsidence of symptoms.
- Symptoms – With evacuation of pus earache will be relieved, Fever decreases.
- Signs – Blood-stained discharge in external auditory canal – becomes mucopurulent, usually associated with small perforations in antero-inferior quadrant of tympanic membrane. The membrane usually returns to normal color.
- Stage of complication
- If the virulence of pathogen is high.
- Disease spreads to acute mastoiditis, sub periosteal abscess, fascial palsy, labyrinthitis etc.
Natural history
- Spontaneous recovery is the usual clinical picture.
- 10% cases discharge happens due to perforation.
- 33% have conductive hearing loss of 20dB at one month after infection, and 20% have it at 3 months.
- Most common complication is acute mastoiditis followed by facial palsy.
- Other Intra temporal / Intra cranial complications.
Investigations
- Tympanometry – to establish middle ear effusion.
- Tympanocentesis & Culture – Rarely required for diagnosis.
- Nasopharyngeal swab for culture and sensitivity.
- Full blood count – Iron deficiency anemia is prone for recurrent acute otitis media.
- Rule out primary ciliary dyskinesia, immuno-compromised states in children with recurrent acute otitis media
- Imaging – CT Scan of mastoid if intracranial complications are suspected.
Treatment of Acute Otitis Media
- 60% of children recover within 24hours with or without treatment, so a watchful waiting may be reasonable in uncomplicated acute otitis media.
- Antibiotic therapy
- Mostly viral etiology, hence antibiotics are not recommended, if giving
- Ampicillin 50mg/kg/day in 4 divided in doses.
- Amoxicillin 40 mg/Kg/day in 3 divided doses.
- Amoxicillin + Clavulanic acid for treatment failures.
- The recent U.S. guidelines recommend.
- 10-day course of therapy for younger children and for children with severe disease.
- 7-day course in children 2 to 5 years of age with mild to moderate acute otitis media
- 5 – 7 days for 6 years of age and older with mild to moderate disease.
- Cephalosporins in cases of penicillin allergy.
- Azithromycin for 1, 3 or 5 days.
- Oral / nasal decongestants
- Ephedrine
- Oxy / Xylometazoline
- Analgesics and antipyretics
- Paracetamol in a dose of 45mg/kg/day in 3 divided doses.
- Ear toilet
- Dry local heat application
- Myringotomy
- Reserved for severe cases where complication is present or suspected, to relieve severe pain or when microbiology is strongly needed.
- Bulging drum
- Persistent effusion > 12 weeks
- Recurrent acute otitis media
- Vaccination
- MMR vaccination
- Against S.pneumoniae – Pneumovax
- Influenza vaccination.
- Adenoidectomy & Tonsillectomy
- Not advised as a first line treatment.
Complications
- Complications can be broadly divided into extracranial and intracranial complications.
- Extracranial
- Tympanic membrane perforation
- Commonest complication
- 0-10% of cases.
- Typically happens in posterior half of Pars Tensa, associated with loss of middle fibrous layer and future posterior retraction pockets.
- Acute mastoiditis
- Disease of childhood.
- 28% less than 1 year age, 38% 1- 4 year, 21% 4 -8year, 8% 8-18years and 4% above 18.
- Myringotomy with or without ventilation tube insertion, culture and sensitivty and intravenous antibiotics are the initial therapy.
- If not resolving, cortical mastoidectomy.
- Acute mastoiditis with periosteitis – when infection spread to periosteum via emissary veins.
- Acute mastoid osteitis and subperiosteal abcess.
- Zygomatic abscess
- Bezolds abscess – Perforation of medial mastoid cortex, tracking down to SCM to posterior triangle.
- Retropharyngeal or parapharyngeal abscess via peritubal cells.
- Masked mastoidits in incompletely treated AOM – Signs may be absent, but otalgia and fever may present.
- Petrositis
- Gradenigo’s Triad – Cranial nerve VI nerve palsy, Pain along Trigeminal Nerve, Otorrhea.
- Management include IV antibiotics, varieties of mastoidectomy ranging from cortical to radical.
- Drainage of petrous apex is no longer recommended.
- Facial Nerve palsy
- Seen in 0.005% cases.
- Responds well to ventilation tube insertion and IV antibiotics.
- Labyrinthitis
- Bacterial toxins enter via round window membrane or preformed pathways like congenital dehiscences, temporal bone fracture lines.
- Serous labyrinthitis – Inflammation of labyrinth without pus formation.
- Suppurative labyrinthitis – Characterized by severe vertigo, nystagmus and permanent hearing loss.
- Treatment ranges from ventilation tube insertion, aggressive intravenous antibiotics, tympanomastoidectomy and cochleotomy.
- Tympanic membrane perforation
- Intracranial complications of Acute Otitis Media
- Persistent headache and fever are most common early symptoms of intracranial complications
- Meningitis is commonest Intracranial complication of AOM
- 50 – 90% cases.
- Younger children, average at 2 years are most commonly affected.
- Treatment is medical line of management.
- If mastoidectomy is needed, it is done only after medical condition improves.
- Extradural abscess
- 2nd most common intracranial complication.
- Pus collects between dura and bone.
- Treatment is surgical drainage.
- Subdural empyema
- Collection of pus between dura and arachnoid membranes.
- Burr hole drainage / craniotomy is advised.
- Sigmoid sinus thrombosis
- Infected thrombus develops within sinus and may then extend proximally or distally to internal jugular vein and superior vena cava entering systemic circulation causing sepsis.
- Headache, Otorrhea, Spiking fever.
- Griesinger’s sign – Mastoid tenderness and edema, secondary to thrombophlebitis of mastoid emissary vein.
- MRI is more sensitive than CT for diagnosis. In CT, the sign of delta appearing as an empty triangle covered with dura contrast in the sigmoid sinus area is typical for sigmoid sinus thrombosis (may not always be observed)
- MRI angiography or arteriography is the gold standard.
- IV antibiotics should be initiated.
- The most frequently used surgical technique is clearing of the surroundings of only sigmoid sinus with surgical drainage of infection.
- Surgical approach to thrombus creates some risks such as septic embolization, expansion towards subarachnoid space, and difficulty in spontaneous recanalization.
- Similar to the way of surgical therapy, the use of heparin or oral anticoagulant agents in sinus thrombosis is controversial.
- Focal otic encephalitis
- Brain abscess
- Persistent headaches are commonest symptom.
- Eventually signs of raised intracranial tension and focal neurological deficits.
- Treatment is by Neurosurgical drainage.
- Otic hydrocephalus
- Complication of AOM manifesting as raised intracranial pressure in absence of any space occupying lesion and without obstruction of CSF.
- Benign intracranial hypertension is synonym.
- Etiology is obscure.
- Headache is predominant symptom.
- MRI is investigation of choice.
- Lumbar puncture and CSF analysis – Normal CSF composition, with elevated CSF pressure.
References
- Önerci, T.M. (2009). Acute Otitis Media. In: Diagnosis in Otorhinolaryngology. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-00499-5_6
- England, R.J., & Shamil, E. (Eds.). (2021). Scott-Brown’s Essential Otorhinolaryngology, Head & Neck Surgery (1st ed.). CRC Press. https://doi.org/10.1201/9781003175995