Retropharyngeal abscess is a potentially life-threatening condition, when infection tracts to lymphoid tissue between posterior pharyngeal wall and prevertebral fascia.
Anatomy of Retropharyngeal space
- The retropharyngeal space lies immediately posterior to posterior pharyngeal wall, extending craniocaudally from the base of the skull to the posterior mediastinum
- Anterior boundary is the buccopharyngeal fascia (visceral fascia)
- Posterior – Alar fascia
- Superior – Skull base
- Inferior – Extends to superior mediastinum, where alar fascia fuses with visceral fascia
- Lateral – bilateral Carotid sheaths with in the parapharyngeal space
- Medial – Midline septum divides retropharyngeal space into two.
- Contents of retropharyngeal space
- Loose areolar tissues and fat.
- Lymph nodes draining lymph nodes that drain the nasopharynx, adenoids, posterior paranasal sinuses, and middle ear. These lymph node chains are present in young children, but atrophy and involute typically by age four to five years old.
Epidemiology & Etiology
- Retropharyngeal space is a rare but serious clinical condition.
- Mainly in infants and young children less than 5 years with a peak incidence between 3 and 4 years due to suppurating retropharyngeal node, following an upper respiratory tract infection.
- Very rarely secondary to penetrated foreign body, or spread of cervical tuberculosis (most common cause in adults).
- Can also cause due to spread of peritonsillar abscess.
- Risk factors for retropharyngeal space infection include poor oral hygiene, diabetes, immunocompromise, and low socioeconomic status.
Sources of infections
- Acute
- Infection in adenoids, nasopharynx, posterior nasal sinuses or nasal cavity
- Penetrating injury / trauma to posterior pharyngeal wall or cervical esophagus
- Petrositis due to acute mastoiditis
- Chronic
- Caries of cervical spine / Pot’s spine
- Tuberculosis of retropharyngeal lymph nodes
- Penetrated foreign body
Bacteriology
- Streptococcus Viridans > S. Aureus > K. pneumoniae > E. coli > Enterobacter > MRSA
Symptoms
- Systemically ill child with fever, irritability, dysphagia (difficulty in swallowing), odynophagia (painful swallowing) and drooling.
- Airway compromise – stridor (noisy breathing)
- Characteristic posture of neck flexed and head extended.
- Neck stiffness, Torticollis
- Hot potato / muffled voice.
- Dribbling and pooling of saliva.
- Chest pain due to mediastinal involvement
Signs
- Bulging posterior pharyngeal wall
- History of Tuberculosis, foreign body, dental problems, intravenous drug abuse.
- Neurological signs due to cord compression.
-
Neck swelling, cervical lymphadenopathy
Differential diagnosis
- Neoplasms – Nasopharyngeal carcinoma, Schwannoma
- Vascular – Aberrant Internal Carotid Artery (ICA), ICA pseudo aneurysm
- Traumatic – Hematoma following whiplash injury
- Infection – Croup, Acute epiglottitis, Parapharyngeal abscess, Peritonsillar abscess,
- Inflammatory – Sarcoidosis, Forestiers disease, Kawasaki disease.
Investigations
- Complete blood count, blood cultures, and preoperative lab tests.
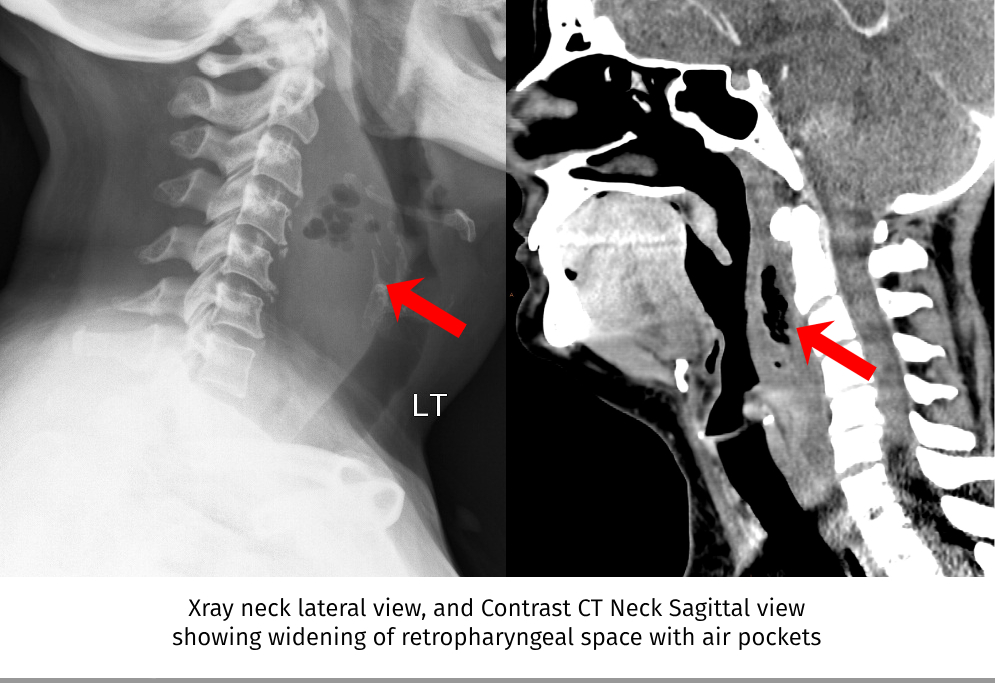
- Lateral X-ray neck
- Shows loss of normal curvature of cervical spine
- Widening of retropharyngeal space.
- Normal width of radiological prevertebral tissue at C2 is 3.5mm. Considered as widened,
- if it is more than 7mm in C2
- more than 14mm in C6 level in children or more than 22 mm at C6 in adults.
- Normal width of radiological prevertebral tissue at C2 is 3.5mm. Considered as widened,
- Chest X-Ray – in patients complaining of chest pain to investigate for mediastinal involvement.
- Ultra sonogram of neck
- Contrast CT of neck is the investigation of choice.
Treatment of Retropharyngeal Abscess
- Retropharyngeal abscess is a surgical emergency.
- Needs hospital admission, intravenous antibiotics, and otolaryngology consultation.
- High dose antibiotic therapy (aerobic and anaerobic coverage) with urgent incision and drainage under general anesthesia is recommended.
- Ampicillin-sulbactam (50 mg/kg every 6 hours) or clindamycin (15 mg/kg every 8 hours) / Vancomycin or linezolid is recommended.
- Usually drained per orally, but occasionally external drainage via neck also done.
- Patient is kept in supine position and head low – vertical incision is made in most fluctuant area of abscess on lateral part of posterior pharyngeal wall with constant suction ready.
- Airway protection by intubation – should be done by a skilled anesthetist; or a tracheostomy may be needed.
- In patients not presenting with severe respiratory distress or airway compromise, a trial of intravenous antibiotic therapy for 24 to 48 hours can be considered with careful airway monitoring, prior to drainage. After 24 to 48 hours of antibiotic therapy, the need for surgical incision and drainage should be reevaluated.
Complications
-
Airway obstruction
-
Sepsis
- Mediastinitis
- Spinal epidural abscess
- Lemierre syndrome – Systemic fusobacterial infection, resulting in IJV thrombophlebitis.
- Osteomyelitis of odontoid process associated with meningitis.
- Acute suppurative thyroiditis.
- Purulent meningitis.
- Twelfth nerve palsy.