Fungal rhinosinusitis (FRS) is a complex and heterogeneous condition, with the role of fungal agents in its pathogenesis remaining incompletely understood. Although fungi can be cultured from the nasal secretions of both healthy individuals and patients with sinus disease, their clinical significance varies. The ability to distinguish between invasive and noninvasive forms of fungal sinusitis is critical, as these subtypes differ in clinical presentation, underlying pathophysiology, and treatment approaches. This distinction is largely based on the presence or absence of fungal hyphae in the sinus mucosa.
Among the fungal species implicated in FRS, Aspergillus is the most common causative agent, followed by Candida and Mucor species. The clinical presentation and severity of FRS can range from mild, noninvasive forms to life-threatening invasive disease. The increasing awareness and recognition of FRS as an important entity have led to advancements in diagnostic methods, classification systems, and management protocols. However, challenges remain in standardizing treatment approaches and addressing high recurrence rates.
Etiology
The etiology of fungal sinusitis is similar to allergic bronchopulmonary aspergillosis (ABPA). Fungal presence in mucous leads to continuous antigenic stimulation, perpetuating an inflammatory response in predisposed individuals.
Pathophysiology
The pathophysiology of fungal sinusitis begins with the inhalation of ubiquitous fungal spores, which serve as an antigenic stimulus. In atopic individuals, this triggers a robust inflammatory response characterized by mucosal edema. The resultant allergic mucin consists of thick green-gray, lamellated material containing eosinophilic inflammatory cells in various stages of degranulation, Charcot-Leyden crystals, and fungal hyphae. This cycle of inflammation and mucin production further exacerbates the condition, leading to persistent sinus pathology.
Classification of Fungal Rhinosinusitis
A widely accepted classification system for FRS is the deShazo classification, which divides fungal sinusitis into distinct clinical entities based on the nature of the disease process. The primary categories include:
1. Allergic Fungal Rhinosinusitis (AFRS)
AFRS is a noninvasive form of fungal sinusitis characterized by a hypersensitivity response to fungal antigens in atopic individuals. Patients typically present with chronic sinus symptoms, including nasal obstruction, nasal discharge, and facial pressure. Thick, eosinophil-rich allergic mucin containing fungal elements is a hallmark feature of AFRS.
Etiology
- Common causative agents: Dematiaceous species (Alternaria, Bipolaris, Curvularia), Aspergillus fumigatus
- Geography: Predominantly in humid areas
- Host factors: Immunocompetent individuals with a history of atopy
Clinical Presentation
- Usually affects young adults
- Bilateral or unilateral nasal obstruction
- Associated with nasal polyps (50% of cases also have asthma)
- “eosinophilic appearing mucin” inside the sinuses
- Symptoms include chronic rhinosinusitis (CRS), pansinusitis, nasal obstruction, proptosis of the eye, and expanded opacities on CT imaging
Immunology
- Elevated Serum IgE levels
- Positive skin tests and Radio Allergen Sorbent Assay (RAST) tests
- Elevated eosinophil count
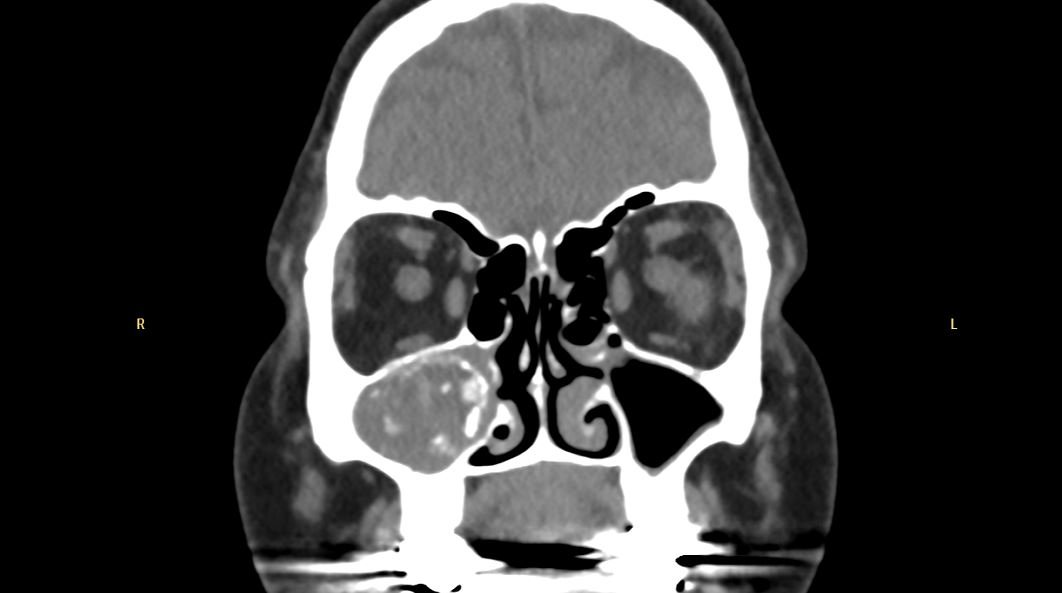
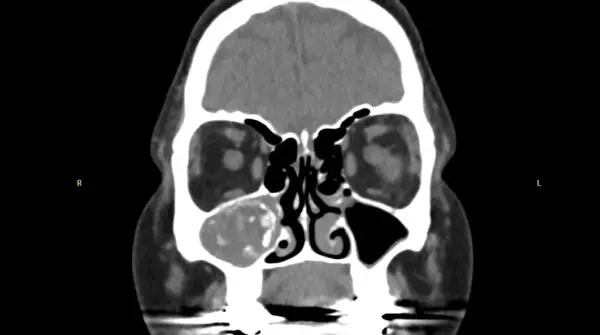
Radiology
- Heterogeneous opacities in CT images
- Bone erosion and deformity in severe cases
Histopathology
- Sparse fungal elements embedded in eosinophilic-rich mucin
- Presence of Charcot-Leyden crystals like those seen in patients with asthma
- No evidence of mucosal or vascular invasion
Diagnosis
Diagnosis is based on clinical data, radiological imaging, immunology, HPE, and mycology. The Bent and Kuhn diagnostic criteria are a set of five criteria used to diagnose AFRS. These criteria were developed in 1994. The five criteria are
- Type 1 hypersensitivity to fungi: Confirmed by history, skin testing, or RAST
- Nasal polyposis: A condition where polyps form in the nose
- Characteristic CT signs: Serpiginous areas of increased attenuation on a computed tomography (CT) scan, unilateral predominance
- Eosinophilic mucus: Mucus with high levels of eosinophils
- Positive fungal stain: A positive fungal stain of sinus contents removed during surgery, Charcot-Leyden crystals, peripheral eosinophilia.
Treatment
- Surgical debridement and aeration (e.g., antrostomy)
- Oral or topical corticosteroids
- Immunotherapy in select cases
Prognosis
- Recurrence is common despite treatment
2. Sinus Fungal Ball (Mycetoma)
A fungal ball, also known as a mycetoma, is a dense collection of fungal hyphae and debris within a sinus cavity. This form of FRS is noninvasive, with no fungal invasion of the mucosa. Patients with fungal balls commonly present with symptoms of chronic sinusitis, such as nasal congestion and facial pain. Radiographic imaging often reveals a hyperdense, calcified lesion within the affected sinus, commonly the maxillary sinus.
Etiology
- Causative agent: Aspergillus species
- Predisposing factors: Chronic sinusitis or previous sinus surgery
Radiology
- Hyperdense, calcified opacity on CT imaging (also called as starry sky pattern)
Treatment
- Surgical removal via endoscopic sinus surgery
- Antifungal therapy is not typically required
3. Acute Fulminant Invasive Fungal Rhinosinusitis
This life-threatening form of FRS occurs primarily in immunocompromised individuals, such as those with uncontrolled diabetes, neutropenia, or undergoing chemotherapy. In acute invasive FRS, fungal hyphae rapidly infiltrate the sinus mucosa, blood vessels, and adjacent tissues, leading to tissue necrosis and potentially fatal complications.
Etiology
- Common agents: Mucorales (Rhizopus, Mucor) and Aspergillus species
- Host factors: Immunocompromised individuals
Clinical Presentation
- Clinicians should have a high index of suspicion for diagnosing invasive fungal sinusitis in patients presenting with
- Rapid onset of facial swelling, numbness or facial pain, and nasal discharge
- Black eschar on the nasal mucosa during nasal endoscopy
- Fever, headache, and visual disturbances
Histopathology
- Vascular invasion and thrombosis with fungal hyphae
- Tissue necrosis
Treatment
- Prompt surgical debridement as the disease is aggressive and with a high mortality rate of around 50%
- Systemic antifungal therapy (e.g., Amphotericin B)
- Correction of underlying immunosuppressive conditions
Prognosis
- High mortality if not promptly treated
4. Chronic Invasive Fungal Rhinosinusitis
Chronic invasive FRS is a slowly progressive condition that primarily affects immunocompetent individuals. It involves fungal invasion of the sinus mucosa and deeper tissues, often leading to fibrosis and granuloma formation over time. Patients may present with persistent facial pain, nasal congestion, and proptosis.
Etiology
- Causative agents: Aspergillus species
- Host factors: Mildly immunocompromised or immunocompetent individuals
Clinical Presentation
- Long-standing symptoms such as facial pain and swelling
- Proptosis and orbital involvement in advanced cases
Treatment
- Surgical debridement
- Prolonged systemic antifungal therapy
Prognosis
- Good with timely intervention but may relapse
5. Granulomatous Invasive Fungal Rhinosinusitis
Granulomatous invasive FRS is a rare form of the disease, characterized by the formation of granulomas and the presence of multinucleated giant cells in response to fungal invasion. This subtype is more common in certain geographical regions, such as South Asia and the Middle East.
Etiology
- Causative agents: Aspergillus flavus
- Geography: Endemic in certain regions
Clinical Presentation
- Chronic progressive disease
- Nasal obstruction, facial swelling, and orbital involvement
Histopathology
- Granuloma formation with multinucleated giant cells
- Sparse fungal elements
Treatment
- Surgical debridement
- Systemic antifungal therapy
Prognosis
- Variable, depending on the extent of the disease.
Summary of types of Fungal Rhinosinusitis
| Type of Fungal Rhinosinusitis | Clinical Data | Radiological Data | Immunology | Histopathology | Mycology |
|---|---|---|---|---|---|
| Allergic fungal rhinosinusitis (AFRS) | Young adults / Nasal obstruction / Polyps | Heterogeneous opacity / Bone erosion | Elevated IgE, Atopic, RAST+ | Eosinophils mucin / Charcot-Leyden crystals | Dematiaceous, Aspergillus |
| Sinus Fungal ball / Mycetoma | Asymptomatic / Postnasal discharge / Headache / Maxillary sinus commonly involved | Opacity of the sinus cavity involved – usually maxillary | Normal | No mucosal invasion | Aero contamination Rare fungal culture, Aspergillus, Scedosporium |
| Acute Invasive fungal rhinosinusitis | Fever / Nasal discharge / Ophthalmic disorders | Tissue infiltration / Bone erosion | Immunocompromise like AIDS or diabetes | Tissue necrosis / Thrombosis | Mucorales / Aspergillus |
| Chronic Invasive fungal rhinosinusitis | Adults / Pain / Proptosis / Neurological symptoms | Tissue infiltration / Bone erosion | Normal | Yes ± granuloma | Miscellaneous Aspergillus |
Treatment in general
Treatment of fungal rhinosinusitis remains controversial and depends on the type of fungal sinusitis. Usual treatment options include
- Removal of All Mucus, Polyps and Fungal debris: Surgical debridement (Functional Endoscopic Sinus Surgery / FESS) is critical. It is both diagnostic and therapeutic. Fungal debris and tissue samples collected during surgery is cultured and mixed with KOH for visualization under a microscope. Histopathology should be done to look for any vascular thrombosis.
- Steroid Therapy: Oral steroids (prednisone) combined with topical intranasal spray will improve symptoms by suppressing inflammation and lowering circulating IgE levels.
- Antifungal Therapy: this includes treatment with Amphotericin B (Polyenes), Itraconazole (Azoles) etc. Systemic antifungals are not ideal therapy for AFRS but can be an adjunct treatment for invasive fungal rhinosinusitis.
- Fungal immunotherapy is also an alternative treatment for AFRS as it can desensitize the body to fungal antibodies.