Atrophic rhinitis (also known as Ozaena) is a progressive, chronic nasal disease defined by mucosal atrophy, bony resorption of the turbinates, and the presence of thick, fetid crusts within the nasal cavity. It is classified into primary and secondary forms based on the presence or absence of identifiable underlying causes.
Etiology of Atrophic Rhinitis
Primary Atrophic Rhinitis
- The exact cause remains unknown.
- Commonly affects females at puberty, suggesting a possible endocrine influence.
- Low socioeconomic status, nutritional deficiencies, particularly iron-deficiency anemia, have been implicated.
- Genetic predisposition and racial susceptibility have been reported, with higher prevalence noted in certain populations (e.g., African Americans).
- An autoimmune mechanism has also been proposed based on the presence of circulating autoantibodies in some patients.
- Infectious agents are postulated to play a contributory role, especially organisms like Klebsiella ozaenae.
Secondary Atrophic Rhinitis
- Occurs due to known precipitating factors such as: Chronic rhinosinusitis, Granulomatous infections like tuberculosis, leprosy, and syphilis Post-surgical sequelae, especially following excessive nasal surgeries or radiation therapy.
Pathophysiology
- Histologically, there is squamous metaplasia of the respiratory epithelium, replacing normal ciliated columnar epithelium with non-keratinized or keratinized squamous epithelium.
- Lamina propria exhibits chronic inflammatory infiltrates, granulation tissue, and fibrosis.
- Mucous glands are reduced in both size and number.
- Vascular changes, including endarteritis and periarteritis of terminal arterioles, contribute to ischemia and atrophy of the turbinates.
- Biochemical analyses have revealed a significant reduction in total phospholipids and altered surfactant composition, suggesting that surfactant deficiency may play a role in disease pathogenesis.
Microbiology
- Multiple organisms have been implicated, particularly:
- Klebsiella ozaenae (now reclassified under Klebsiella pneumoniae subsp. ozaenae)
- Diphtheroid bacilli
- Bordetella bronchiseptica
- Pasteurella multocida
- Anaerobic flora are believed to contribute significantly to the malodor.
Clinical Features of Atrophic Rhinitis
- Foul smell (ozaena) due to anaerobic colonization.
- Anosmia is common and may paradoxically provide relief to the patient (“merciful anosmia”).
- Nasal obstruction from crusting, despite an anatomically wide nasal cavity.
- Headache, epistaxis, and facial discomfort may occur.
- Maggots (myiasis) may rarely be seen in neglected cases.
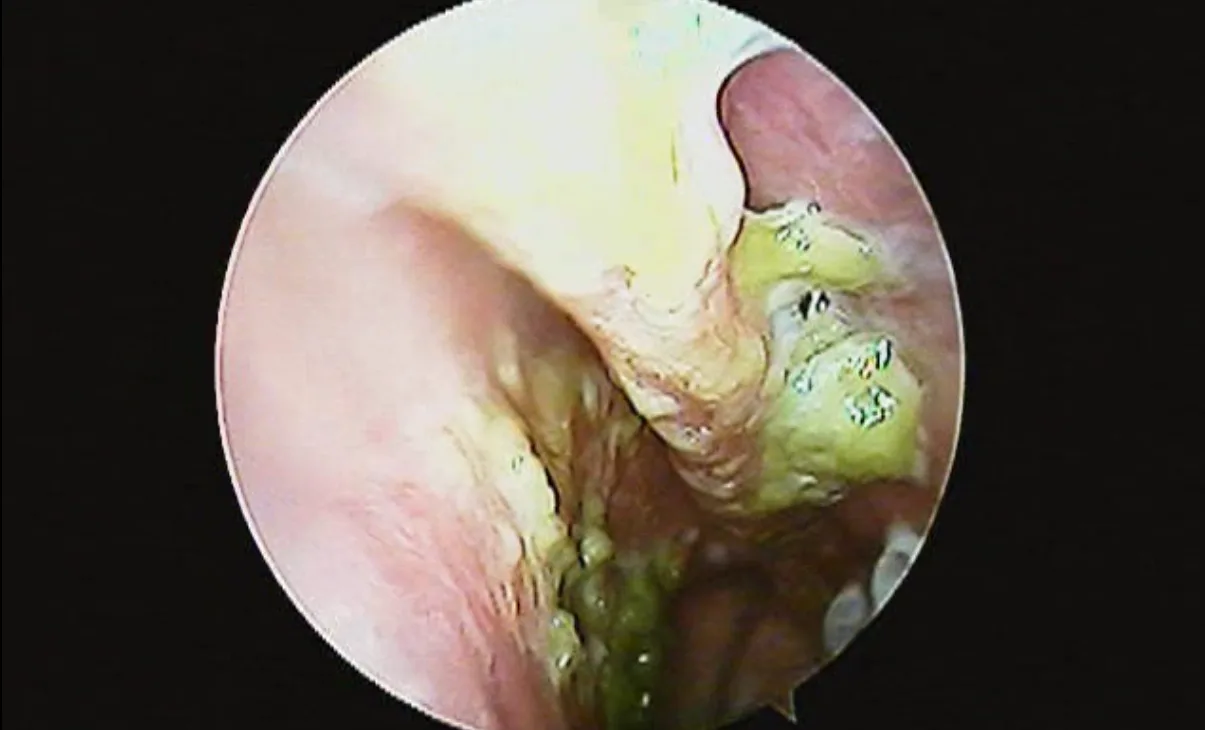
- Diagnostic nasal endoscopy will show typical crusting: Brown to black or green crusts, predominantly in the posterior nasal cavity.
- Septal perforation and nasal saddling are uncommon.
- Associated symptoms include pharyngitis sicca, and if the larynx is involved, hoarseness and dry cough (atrophic laryngitis).
Imaging
- CT scans or X-rays of the paranasal sinuses reveal hypoplastic sinuses with thickened bony walls, consistent with arrested sinus development. This makes procedures like antral puncture technically challenging.
Investigations
- Nasal swab cultures for microbiological analysis.
- Serologic tests to exclude syphilis and other granulomatous diseases.
- Complete blood count, serum iron, and protein levels to assess nutritional status.
- Radiological imaging to evaluate sinus development and rule out chronic rhinosinusitis.
Treatment of Atrophic Rhinitis
Medical Treatment
- Nasal douching with alkaline solutions (e.g., A mixture of Sodium Bicarbonate, Sodium Biborate, and common salt in 1:1:2 ratio dissolved in 280 mL water) twice daily to aid in crust removal.
- Topical application of 25% glucose in glycerine post-douching to reduce bacterial colonization by inhibiting proteolytic enzymes.
- Rifampicin 600 mg once daily for 12 weeks has demonstrated bacteriological and clinical improvement in some studies.
- Human placental extract injections have shown anecdotal benefit in mucosal regeneration.
Surgical Treatment
- Indicated in patients with poor compliance or failure of medical management.
- Young’s Operation: Complete closure of the nasal cavity using flaps from the vestibule to prevent airflow, allowing mucosal healing. The nasal cavity is reopened after 6–12 months.
- Modified Young’s Operation: Similar to the original procedure but leaves a small (approx. 3 mm) central opening to preserve minimal airflow and minimize morbidity.
- Ghosh Operation: Vestibuloplasty involving a posteriorly based skin flap on the lateral vestibular wall, aiming to reduce nasal airflow without full closure.
- Historical methods involving paraffin, Teflon, plastipore, cartilage grafts, etc., are largely obsolete.
Recent Scientific Advances in Atrophic Rhinitis
- Platelet-Rich Plasma (PRP) Therapy
PRP therapy involves the submucosal injection of autologous platelet-rich plasma, which is rich in growth factors and cytokines. These components promote tissue healing and regeneration. Clinical studies have demonstrated that PRP can effectively reverse mucosal atrophy and reduce crusting in AR patients. It is emerging as a promising biological treatment modality for AR. - Nasal Microbiome Modulation with Manuka Honey
Recent studies have highlighted the role of nasal microbiota dysbiosis in the pathogenesis of AR. Topical application of 10% manuka honey has been shown to restore microbial balance, reduce inflammation, and promote mucosal healing. Patients treated with manuka honey exhibited significant clinical improvements, including decreased crusting and nasal discharge. - Bioactive Glass Implants
A novel surgical approach involves the sublabial implantation of bioactive glass particles to reconstruct atrophic nasal turbinates. This technique aims to restore nasal airflow dynamics and mucosal function, offering a less invasive alternative to traditional surgical methods. - Tissue Engineering and Regenerative Medicine
Advancements in tissue engineering, including the use of seed cells, scaffold materials, and growth factors, are being explored to regenerate normal nasal mucosa and reconstruct atrophic turbinates. Emerging technologies like 3D printing and organoids hold potential for developing personalized treatments for AR.
Atrophic rhinitis remains a challenging condition due to its obscure etiology and chronicity. A combination of targeted medical therapy and surgical intervention, guided by symptom severity and patient compliance, offers the best outcomes. Further research is warranted into the autoimmune and biochemical mechanisms of the disease to develop novel therapeutic options.
References
- El-Anwar MW, Nofal AA, Foad YS, Khallaf HS. Platelet rich plasma injection in treatment of primary atrophic rhinitis. Egypt J Hosp Med. 2019;74(5):1076–80.
- Elnashar IS, Abdel Aziz AM, Ramadan ZA. Efficacy of platelet-rich plasma in treatment of primary atrophic rhinitis: Randomized controlled trial. Egypt J Otolaryngol. 2020;36:4.
- Mohammad TR, Alyahya KA, Almutairi HR. Effect of topical manuka honey in patients with atrophic rhinitis. Microorganisms. 2022;10(11):2092.
- Mandal A, Jaiswal AA, Venkatesh MG, Sinha S, Thomas L, Rajeshwari A. Bioactive glass sublabial implantation for primary atrophic rhinitis: A novel approach. Laryngoscope Investig Otolaryngol. 2022;7(5):1269–76.
- Li H, Pan Y, Wang X, Zhang J, Xiong X, Liu J. Advances in tissue-engineered nasal mucosa: From basic science to clinical translation. Front Bioeng Biotechnol. 2023;11:1182605.