Facial nerve (FN) (the nerve which is responsible for the facial expression) dysfunction presents with a spectrum of deficits ranging from subtle weakness to complete paralysis.
Accurate grading is essential for prognosis, documentation, research comparison, and monitoring recovery or degeneration.
Several grading and assessment systems have been proposed for grading facial nerve dysfunction, each with distinctive advantages and limitations. This article outlines the major systems, compares their usefulness, and summarizes their clinical utility.
1. Classic Objective and Semi-Objective Systems
1.1 Burres & Fisch System
The Burres–Fisch system is one of the earliest attempts to quantify facial nerve dysfunction using linear measurements of facial movements.
Key Features
- Objective system based on standardized measurements of facial landmarks.
- Records oral commissure excursion, palpebral fissure width, nasolabial fold depth, etc.
- Provides an overall score for facial symmetry and movement.
- Particularly useful in research settings requiring precise numeric comparisons.
Limitations
- Time-consuming.
- Requires photographic documentation and careful calibration.
- Less practical for routine clinical use.
1.2. Nottingham System
The Nottingham grading system employs subjective assessment of movement across several facial points.
Key Features
- Clinically simple and does not require equipments.
- Each region—forehead, eyes, nasolabial fold, lips—is graded individually.
- Total score provides overall FN function.
Limitations
- Less precise in partial paralysis or synkinesis.
1.3. Neely System (Computer-Assisted Image Analysis)
Neely introduced a computer-based image processing system for facial motion quantification.
Key Features
- Uses high-resolution video and software to analyze: Facial landmarks, Excursion vectors, Symmetry indices.
- Highly objective and reproducible.
- Useful for research and facial reanimation outcome analysis.
Limitations
- Requires specialized software and equipment.
- Not widely available for routine practice.
1.4. Johnson & Jansen Methods (Objective Branch-Level Assessment)
These systems focus on individual peripheral branches of the facial nerve.
Key Features
- Enables analysis of zygomatic, buccal, marginal mandibular, and cervical branch movement.
- Useful when paralysis is partial or localized.
- Provides a “regional” rather than “global” picture.
Limitations
- Not a standardized global scoring system.
- Mainly used in research on surgical outcomes or nerve repair.
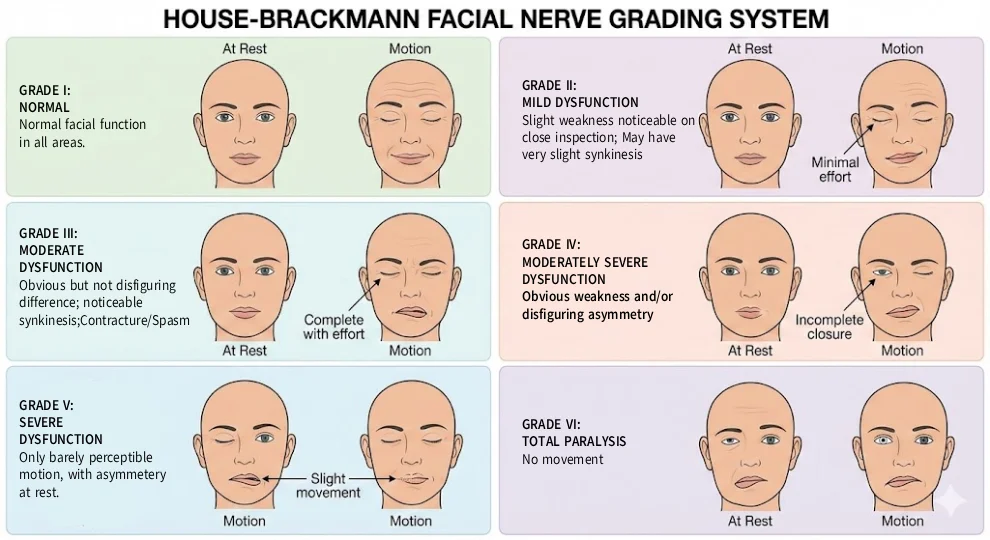
2. House–Brackmann (HB) Facial Nerve Dysfunction Grading System
The House-Brackmann scale, published in 1985, is the most widely used global grading system today.
Advantages
- Simple, quick, reproducible in clinical settings.
- Provides global assessment of facial function.
- Good for:
- Bell’s palsy,
- Acute facial nerve injuries,
- Evaluating recovery in neuropraxia and axonotmesis.
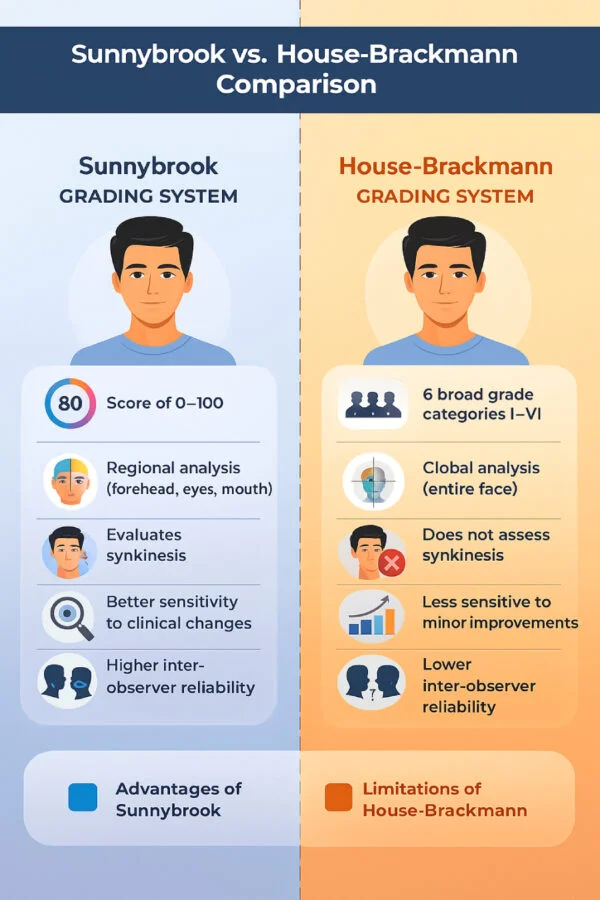
Disadvantages
- Inter-observer and intra-observer variability.
- Not precise enough for:
- Synkinesis grading,
- Branch-level assessment,
- Post-repair evaluation.
- Not useful in transected or grafted nerves, because:
- Repairs produce mass movements and synkinesis
- Most patients regain eye closure and oral competence.
- Forehead movement rarely recovers.
When HB Works Best: Only when the nerve sheath is intact or injury is Sunderland grade I–IV.
| Grade | Description | Characteristics | ||||
| Gross | At rest | Motion | ||||
| Forehead | Eye closure | Mouth | ||||
| I | Normal | Normal facial function in all areas | ||||
| II | Mild dysfunction | Slight weakness noticeable on close inspection May have very slight synkinesis | Normal symmetry and tone
| Moderate to good function | Complete closure with minimum effort | Slight asymmetry |
| III | Moderate dysfunction | Obvious but not disfiguring difference between two sides; Noticeable but not severe synkinesis Contracture and/or hemifacial spasm | Normal symmetry and tone | Slight to moderate movement | Complete closure with effort | Slightly weak with maximum effort |
| IV | Moderately severe dysfunction | Obvious weakness and/or disfiguring asymmetry | Normal symmetry and tone | None | Incomplete closure | Asymmetric with maximum effort |
| V | Severe dysfunction | Only barely perceptible motion | Asymmetry | None | Incomplete closure | Slight movement |
| VI | Total paralysis | No movement | ||||
3. Modern Facial Nerve Grading Systems
3.1 Sunnybrook Facial Grading System (SFGS)
One of the most widely endorsed modern systems. The tool objectively assess and grade the severity of facial palsy by comparing the affected side of the face to the healthy side. It uses a 0–100% composite score and evaluates three main areas: resting symmetry, voluntary movement, and synkinesis (involuntary movement).
Components
- Resting symmetry
- Voluntary movement (5 regions)
- Synkinesis (during smile, eye closure, lip pucker)
Output
- Composite score 0 to 100.
Strengths
- More sensitive to clinical change than HB
- Includes synkinesis
- Better inter-observer reliability
- Regional analysis gives granular detail
- Provides a quantitative way to track recovery and response to treatment over time.
- It is now the preferred tool in:
- Facial reanimation surgery outcomes
- Synkinesis rehabilitation
- Research trials
3.2 FaCE Scale (Facial Clinimetric Evaluation)
A patient-reported outcome measure, complementary to clinician grading.
It was developed by Dr. Jeffrey B. Kahn and colleagues in order to measure both impairment and disability associated with facial dysfunction. It can specifically assess facial function and quality of life after facial paralysis.
Domains
- Facial movement
- Oral function
- Eye comfort
- Facial comfort
- Social function
- Social well-being
- Strengths
Captures psychosocial burden of FN dysfunction. Essential for outcome studies in cosmetic and reanimation procedures.
3.3 eFACE (Electronic Facial Assessment Tool)
A validated digital, smartphone/tablet-based system.
Features
- Generates continuous numeric scores for:
- Static symmetry
- Dynamic movement
- Synkinesis
Strengths
- High reproducibility
- Ideal for telemedicine
- Becoming a research standard (Hadlock et al.)
4. Assessment of Synkinesis
Synkinesis is common after facial nerve regeneration and is poorly captured by HB.
Useful tools include:
- Synkinesis Assessment Tools
- Sunnybrook synkinesis subscore
- eFACE synkinesis component
- Synkinesis Assessment Questionnaire (SAQ)
- Terzis synkinesis classification
Key Synkinesis Patterns
- Ocular–oral
- Oral–ocular
- Platysmal overactivation
- Mentalis contraction
Inclusion of synkinesis is mandatory for modern FN assessment.
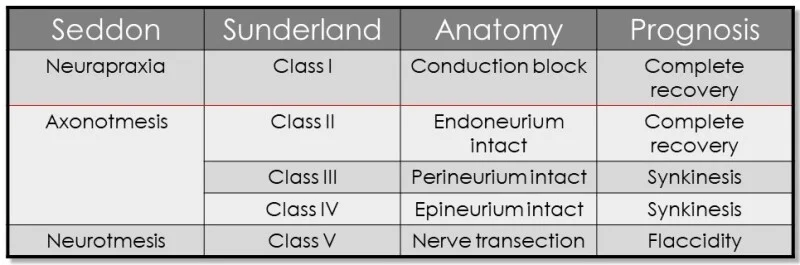
5. Nerve Injury Classification Systems
Understanding the type of nerve injury guides prognosis and determines which grading systems are applicable.
5.1 Seddon Classification
- Neuropraxia – Reversible blockage of transmission of nerve impulses due to pressure on nerve fibers. Release of pressure results in rapid and complete recovery of function with no distal Wallerain degeneration.
- Axonotmesis – Involves blockage of axoplasmic flow. Though endoneural tubules are preserved, distal Wallerian degeneration happens.
- Neurotmesis – Complete nerve transection. Wallerian degeneration happens over a 3-4 days’ time.
5.2 Sunderland Classification (I–V)
The Sunderland classification is a widely used system for grading the severity of peripheral nerve injuries into five degrees based on the specific anatomical structures damaged, which helps determine prognosis and treatment.
- First degree
- Reversible
- Allows complete recovery which begins in 1-4 weeks.
- Corresponds to HB Grade I
- Second degree
- Wallerian degeneration occurs, but endoneurial architecture is preserved.
- Recovery is usually complete starts in 1-2 months
- Corresponds to HB Grade II
- Third degree
- Wallerian degeneration and disruption of endoneurial architecture is occurs.
- Recovery is incomplete with functional deficit usually starts by 2-4 months
- Corresponds to HB Grade III-IV
- Fourth degree
- Significant nerve injury.
- Only epineurium is intact.
- Recovery is poor starts by 4-18 months.
- Corresponds to HB Grade V
- Fifth degree
- Complete and total disruption of nerve continuity.
- No recovery without surgical intervention.
- Corresponds to HB Grade VI
Disadvantage
- Only applicable to traumatic injuries of peripheral nerve and not to viral, inflammatory or infiltrative lesions.
Clinical relevance:
- HB is valid only for Grades I–IV
- Grades V require nerve repair → HB not suitable → use RFNRS
6. Repaired Facial Nerve Recovery Scale (RFNRS) – Gidley et al.
House-Brackmann scale fails in cases of nerve repair because, repairs often lead to: Synkinesis, Mass movement patterns, Loss of independent forehead movement etc.
Hence RFNRS was designed specifically for nerve repairs such as neurorrhaphy and interposition grafts. RFNRS categorizes recovery using letters (A–F).
| Repaired Facial Nerve Recovery Scale – Gidley et al | |
| Score | Function |
| A | Normal facial function |
| B | Independent movement of eyelids and mouth, slight mass motion, slight movement of forehead |
| C | Strong closure of eyelids and oral sphincter, some mass motion, no forehead movement |
| D | Incomplete closure of eyelids, significant mass motion, good tone |
| E | Minimal movement in any branch, poor tone |
| F | No movement |
Conclusion
Multiple grading systems exist for FN dysfunction, each addressing different clinical needs.
- House–Brackmann remains globally used but limited.
- Sunnybrook and eFACE offer superior modern assessment with synkinesis evaluation.
- FaCE scale captures patient-reported outcomes.
- RFNRS is essential for repaired nerves.
- Sunderland/Seddon classifications and ENoG/EMG refine prognosis.
A comprehensive evaluation of facial nerve dysfunction is best achieved using a combination of clinical grading, synkinesis scoring, patient-reported outcomes, and electrophysiologic tools.
References
- Burres SA, Fisch U. The comparison of facial nerve grading systems. Otolaryngol Clin North Am. 1982.
- Murty GE et al. The Nottingham system: Objective assessment of facial nerve function. Clin Otolaryngol. 1994.
- Neely JG et al. Computer-assisted facial motion analysis. Otolaryngol Head Neck Surg. 1992.
- Johnson PC et al. Objective facial movement analysis. Arch Otolaryngol.
- Jansen C et al. Regional facial nerve assessment. Laryngoscope.
- Banks CA, et al. Clinician-Graded Electronic Facial Paralysis Assessment: The eFACE. Plast Reconstr Surg. 2015.
- House JW, Brackmann DE. Facial nerve grading system. Otolaryngol Head Neck Surg. 1985.
- Gidley PW et al. Repaired Facial Nerve Recovery Scale. Arch Otolaryngol Head Neck Surg.