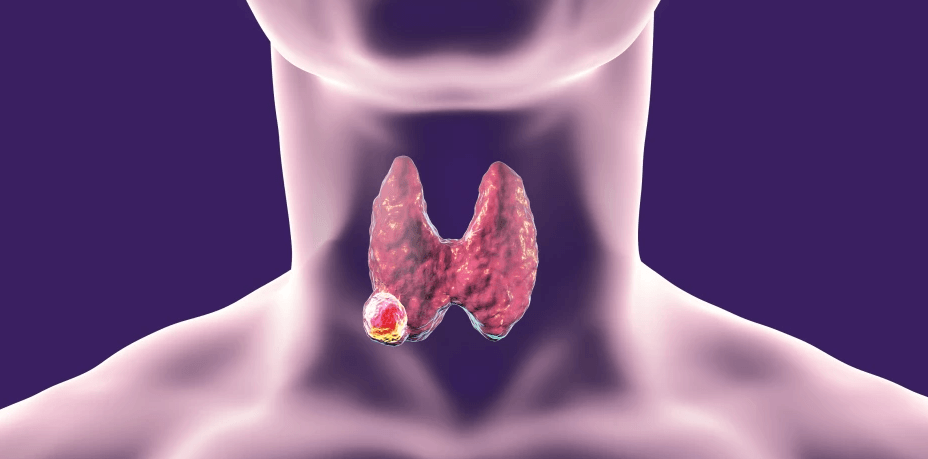
Papillary carcinoma thyroid (PTC) is the most common type of thyroid malignancy but carries the best overall prognosis.
PTC is generally well-differentiated and slow-growing, often presenting as a solitary thyroid nodule (STN). Despite its indolent nature, it frequently exhibits cervical lymph node metastases and, in some cases, pulmonary metastases at the time of diagnosis.
Epidemiology
- Accounting for 60-80% of all thyroid malignancies.
- In a report based on the Surveillance, Epidemiology, and End Results (SEER) database from 1975 to 2012, the incidence of PTC increased from 4.8 to 14.9 per 100,000
- It predominantly affects young adults aged 30-49 years, with a female-to-male ratio of 3:1.
- It is also the most common thyroid cancer in children.
Etiology
The exact cause of PTC is not fully understood, but multiple risk factors contribute to its development:
- Radiation Exposure: Ionizing radiation exposure, particularly during childhood, significantly increases the risk of developing PTC. This includes therapeutic radiation and environmental exposure, such as fallout from nuclear accidents (e.g., Chornobyl disaster).
- Genetic Factors: Familial cases of PTC account for about 5% of cases and may involve syndromes such as familial adenomatous polyposis (Gardner syndrome), Werner syndrome, and Carney complex type 1. Chromosomal rearrangements have been identified in PTC, including the RET protooncogene, NTRK1, and MET gene overexpression. Mutations in the BRAF gene have also been identified and correlated with prognosis, particularly BRAFV600E mutation.
- Dietary Iodine Levels: Both excessive and deficient iodine intake have been implicated in thyroid carcinogenesis.
- Preexisting Thyroid Disease: Conditions like multinodular goiter and Hashimoto’s thyroiditis have been associated with an increased risk of PTC.
- Obesity and Hormonal Factors: A rising incidence of thyroid cancer has been linked to obesity and metabolic syndrome.
Clinical Presentation
- PTC typically manifests as a painless, slowly enlarging thyroid nodule, with an average size of 1.5 cm at diagnosis.
- It is multifocal in 80% of cases and bilateral in 10%.
- The primary tumor may be impalpable, and in such cases, the initial presentation may be with cervical lymphadenopathy.
- Hoarseness and dysphagia occur in approximately 20% of cases, indicating recurrent laryngeal nerve involvement with vocal cord paralysis or tracheal compression.
- Cervical nodal metastases to levels III-VII occur in approximately 70% of cases, while 20% of patients present with pulmonary metastases.
- On palpation, it is painless hard lesion with a rubbery consistency.
Woolner Classification of Papillary carcinoma Thyroid
PTC can be classified based on its extent of involvement:
- Occult Sclerosing: Appears as an irregular white scar within a normal or goitrous thyroid gland; often an incidental finding (4-30% at autopsy). Despite its higher incidence, the prognosis remains favorable.
- Minimal/Microcarcinoma: Tumor diameter <1.0 cm.
- Intrathyroidal: Tumor >1.0 cm but confined to the thyroid gland.
- Extrathyroidal: Tumor extends beyond the thyroid capsule and/or has lymph node metastases.
Investigations
- Ultrasonography (USG): Hypoechoic nodule with irregular margins, micro-calcifications, taller-than-wide shape, and disorganized internal vascularity. TIRADS Classification helps in assessing further evaluation of the nodules
- Fine Needle Aspiration Cytology (FNAC): It is frequently the initial diagnostic method used in the detection of PTC.
- Computed Tomography (CT): Solid lesions with cystic components and punctate or amorphous calcifications. Contrast enhanced imaging also helps in identification of lymph node metastasis.
- Magnetic Resonance Imaging (MRI): Isointense on T1-weighted imaging (T1WI) and iso/hyperintense on T2-weighted imaging (T2WI).
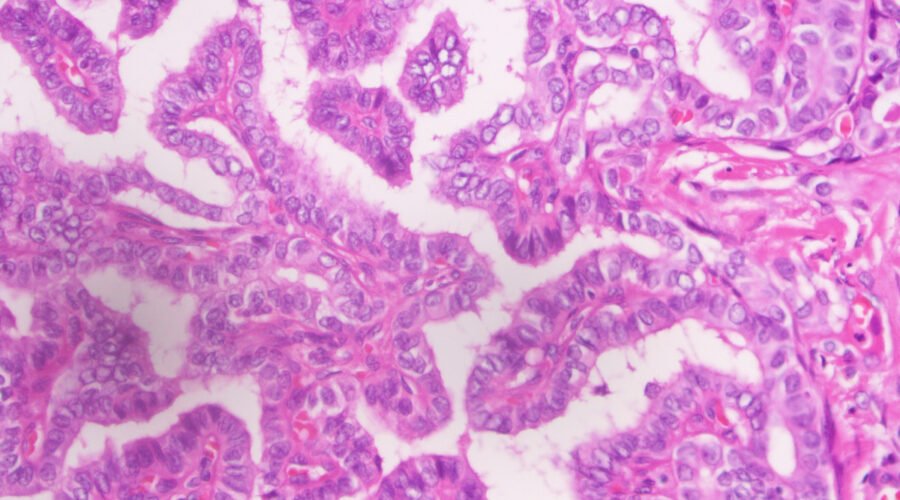
Histopathology
- Macroscopic Features: Firm, unencapsulated tumor that is well circumscribed within the normal thyroid tissue.
- Microscopic Variants
- Pure Papillary: Rare variant.
- Mixed Papillary-Follicular (Tall Cell and Columnar Cell Variants): The most common type. More aggressive, larger tumors with frequent vascular and extrathyroidal invasion. Poor prognosis, especially in older patients.
- Follicular Variant of PTC: The papillary component consists of fibrous stalks surrounded by follicular epithelium.
- Characteristic Features:
- Psammoma Bodies: Laminated calcifications found in stalk regions.
- Orphan Annie Nuclei: Clear, ground-glass nuclei, a hallmark of PTC.
Treatment (Based on 2015 ATA Guidelines)
Risk stratification in PTC is essential for determining prognosis and guiding treatment. The American Thyroid Association (ATA) Risk Stratification System classifies patients into three categories based on clinical, pathological, and molecular factors:
- Low-Risk PTC (Tumors ≤4 cm, No Extrathyroidal Extension, No Distant Metastases):
- Lobectomy is preferred for unifocal tumors ≤4 cm without lymph node metastases.
- Total Thyroidectomy for tumors >4 cm or with bilateral/multifocal disease.
- TSH suppression therapy with levothyroxine to reduce recurrence risk.
- Intermediate-Risk PTC (Minimal Extrathyroidal Extension, Lymph Node Metastases, Aggressive Histology):
- Total Thyroidectomy is recommended. Radioactive Iodine (RAI) Therapy may be considered based on risk stratification.
- TSH suppression therapy to achieve serum TSH <0.1 mU/L.
- High-Risk PTC (Gross Extrathyroidal Extension, Distant Metastases, Incomplete Resection):
- Total Thyroidectomy with Central/Lateral Neck Dissection as needed.
- RAI Therapy for remnant ablation and metastatic disease treatment.
- TSH suppression therapy to maintain TSH levels <0.1 mU/L.
- Consider external beam radiation therapy (EBRT) for unresectable or locally invasive tumors.
- PTC in Thyroglossal Duct Cyst:
- If completely excised via Sistrunk’s procedure with no additional disease: TSH suppression and serum thyroglobulin monitoring.
- If residual disease is suspected: Total Thyroidectomy with RAI Therapy.
Micro papillary cancers can be followed conservatively with active surveillance and without any intervention, and surgery can be pursued only if there is a significant change in size or internal features of the tumor. If surgery is chosen for patients with thyroid cancer <1 cm without extra-thyroidal extension and cN0, the initial surgical procedure should be a thyroid lobectomy unless there are clear indications to remove the contralateral lobe.
Prophylactic central-compartment neck dissection (ipsilateral or bilateral) should be considered in patients with PTC with clinically uninvolved central neck lymph nodes (cN0) who have advanced primary tumors (T3 or T4) or clinically involved lateral neck nodes (cN1b) or if the information be used to plan further steps in therapy.
The decision on type of thyroidectomy depends on various factors. You can watch the following presentation about thyroidectomy for more information.
Adjuvant Treatment and Follow up
Adjuvant Radioiodine Therapy
After thyroidectomy, radioiodine is the therapy of choice in patients with PTC to ablate residual normal thyroid tissue. It is considered in several cases:
- Patients with a tumor >2 cm and 1 of the following risk factors: gross extra-thyroidal extension, age >45 years, lymph node and distant metastases.
- Patients with a tumor <2 cm and distant metastasis.
Radioactive iodine therapy is given 4 to 6 weeks after surgery. Before treatment, a hypothyroid state is induced by stopping thyroid hormone replacement treatment. The therapy is continued until no more radioactive iodine uptake is seen.
Potential adverse effects of radioactive iodine include:
- Sialoadenitis,
- Pulmonary fibrosis,
- Emesis,
- Brain edema (can be prevented with the use of corticosteroids)
- Infertility
- There is a small risk of leukemia, breast, or bladder cancer.
Thyroid Hormone Treatment
After thyroidectomy, patients require lifelong thyroid hormone therapy, usually as monotherapy with levothyroxine (LT4). Since TSH can promote the growth of remaining PTC cells, the dosage of LT4 should initially be high enough to achieve suppression of thyrotropin based on the dynamic risk stratification.
The thyroid function should be checked after 6 to 8 weeks. Depending on the result, the dosage should be adjusted; the use of TSH suppressive therapy should merit careful consideration since it carries an increased risk of complications.
Long-term follow up is necessary every 6 to 12 months for at least 5 years and annually thereafter to look for recurrence. During those visits, TSH, thyroglobulin, and antithyroglobulin antibodies should be measured.
Prognosis of Papillary Carcinoma Thyroid
PTC generally has an excellent prognosis. Poor prognostic factors of PTC include:
- Older age at diagnosis, Large tumor size, Extra-thyroidal growth, Male sex, Less differentiated or solid areas, vascular invasion, and aneuploid cell population.
- Those with aggressive histology
- Extra-thyroidal extension occurs in 8% to 32% of the cases.
- Cervical Lymph Node Involvement: Common (70%), but does not significantly affect prognosis except in the elderly.
- Aggressive Disease in Elderly: Higher risk of invasion into the larynx and trachea, leading to poor prognosis.
- Local or regional recurrences occur in 5 to 15% of patients with PTC.
- Distant Metastases: Lung and bone metastases occur in 5-7% of cases, with 20% of patients having pulmonary metastases at presentation. Other less common sites are the brain, liver, and skin.
- Survival Rates:
- 10-year survival for low-risk PTC: >95%.
- 10-year survival for high-risk PTC: ~60%.
- Overall – 96% survival rate at 5 years, 93% at 10 years, and >90% at 20 years
Papillary carcinoma of the thyroid is a common and well-differentiated malignancy with a favorable prognosis. Early detection through imaging and histopathological evaluation, coupled with appropriate surgical, radioiodine, and TSH suppression therapy per ATA guidelines, ensures excellent long-term outcomes. Regular follow-up with thyroglobulin monitoring and risk stratification is essential for disease surveillance and early detection of recurrence.