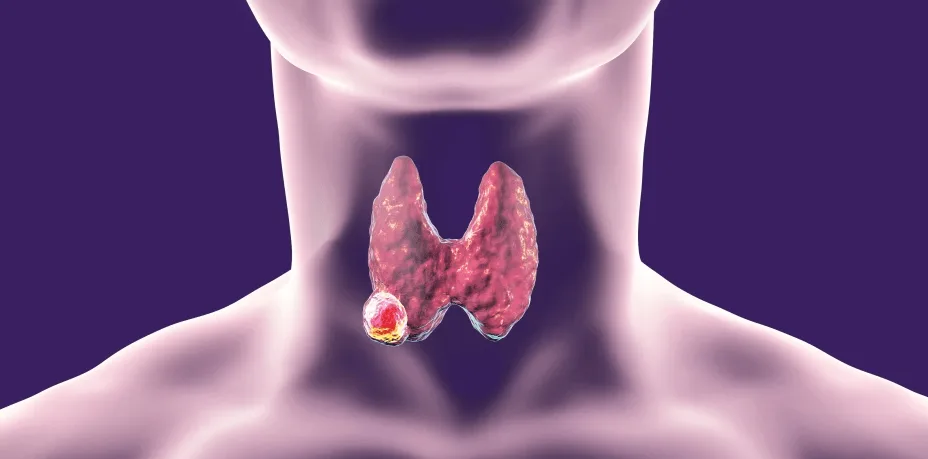
Anaplastic thyroid cancer (ATC) represents one of the most lethal human malignancies. It comprises only 1–2% of thyroid cancers but accounts for nearly half of all thyroid cancer–related deaths. The annual age-adjusted incidence is approximately 1–2 cases per million individuals.
ATC predominantly affects individuals in their sixth to seventh decade, with female predominance.
The etiology of ATC remains poorly understood. Approximately 20% of cases are associated with a history of differentiated thyroid carcinoma or long-standing multinodular goiter. Dedifferentiation of well-differentiated thyroid cancers into ATC is considered a plausible mechanism, supported by molecular evidence of shared mutations such as BRAF and TERT promoter alterations.
Clinical Presentation
- Its presentation is dramatic, with rapidly enlarging anterior neck mass and early invasion of airway, adjacent structures and even distant metastasis.
- Mostly it presents as rapid enlargement of a longstanding goiter, associated with otalgia (ear ache), hoarseness (voice change), stridor (breathing difficulty), airway compromise. But in some patients, it may be spontaneous (without any pre-existing thyroid pathologies).
- Common features include:
- Neck mass: Hard, fixed, irregular (“craggy”) consistency with positive Berry’s sign (tracheal invasion).
- Compressive symptoms: Dysphagia, dyspnea, stridor, hoarseness, and airway compromise.
- Referred symptoms: Otalgia and painful neck swelling in some patients.
- Metastatic disease: Cervical lymph node involvement in ~40% of patients; distant metastases (lungs, bone, brain) are frequent at diagnosis.
- Airway obstruction is often the most urgent clinical problem requiring immediate evaluation and management.
Diagnostic Workup
- Laboratory tests:
- Thyroid function tests (TFTs): usually normal.
- Serum calcitonin and CEA: mainly for excluding medullary thyroid carcinoma.
- Imaging
- Ultrasound neck: Useful for evaluating thyroid lesions and cervical lymph nodes.
- Cross-sectional imaging: All patients should be staged with a 18-fluorodeoxyglucose (FDG) positron emission tomography (PET) scan or Contrast-enhanced computed tomography (CECT) scan of the brain, neck, chest, abdomen, and pelvis.
- Tissue diagnosis:
- Fine-needle aspiration cytology (FNAC) or core needle (Trucut) biopsy confirms undifferentiated malignancy.
- Histology: ATC lacks organized architecture or resemblance to thyroid follicular cells. Spindle cell / sarcomatoid variant, giant cell variant, and epithelial / small cell variants are the three different types, of which spindle/giant cell variants are more common..
- Immunohistochemistry: Negative for TTF-1 and thyroglobulin; PAX8 positive in ~50%; frequent high PD-L1 expression.
- Endoscopic evaluation
- Flexible laryngoscopy: Recommended in all patients to assess vocal cord mobility, as recurrent laryngeal nerve invasion is common.
- Bronchoscopy: Indicated when airway invasion is strongly suspected.
- Molecular testing
- Next-generation sequencing (NGS) should be performed urgently to identify actionable targets (BRAF V600E, RET and NTRK fusions, TERT, TP53, ALK, PD-L1 expression).
Differential Diagnosis
- Key considerations: Lymphoma (curable, urgent distinction), sarcoma, spindle-cell medullary carcinoma, and metastatic disease. Immunohistochemistry and clinical context are essential.
Treatment of Anaplastic Thyroid Cancer
- Staging of thyroid carcinoma follows the AJCC 8th edition system, in which all cases of anaplastic thyroid cancers are considered stage IV because of the aggressive tumor biology.
- Stage IVA: Tumor confined to the thyroid.
- Stage IVB: Tumor extends beyond the thyroid but without distant metastasis.
- Stage IVC: Distant metastatic disease present.
- All patients with anaplastic thyroid cancer should be assessed for systemic disease prior to starting the treatment.
Traditional Approaches
Surgery: Complete surgical resection remains the only potential curative option in patients with localized anaplastic thyroid carcinoma. Current recommendations favor total thyroidectomy with therapeutic lymph node dissection, with en bloc resection of adjacent structures when feasible. The primary objective is to achieve negative surgical margins. However, in most cases, curative surgery is not feasible because of the tumor’s early and extensive infiltration into vital cervical structures.
Traditionally, resection has been limited to palliation or to the small subset of patients with potentially resectable disease. Neoadjuvant targeted therapy (e.g., dabrafenib + trametinib for BRAF V600E–mutated tumors) may downstage disease and facilitate curative resection.
Radioiodine: Ineffective, as ATC lacks iodine uptake.
Radiotherapy: External beam radiotherapy (EBRT) is commonly advised after resection and, when combined with concurrent systemic therapy, offers improved overall survival compared with monotherapy. Intensity-modulated radiation therapy (IMRT) is now preferred, as it enhances local control while limiting toxicity to surrounding structures.
Nevertheless, early recurrence remains a challenge, and median survival after EBRT is typically 6–12 months, though recent studies suggest selected patients treated with trimodality approaches (surgery, chemoradiation, and targeted therapy) may achieve extended survival beyond one year.
Chemotherapy: Historically disappointing; agents used include doxorubicin, cisplatin, paclitaxel—usually without durable benefit
Evolving Paradigms: Molecularly Targeted & Immunotherapy
Molecular profiling has become central to the modern management of anaplastic thyroid carcinoma. Identification of actionable mutations allows for the use of targeted therapies and immunotherapy, which have significantly altered outcomes in selected patients.
- BRAF V600E Mutations (~35–40% of ATC cases)
- Agents: Dabrafenib (BRAF inhibitor) + Trametinib (MEK inhibitor).
- Evidence: The ROAR basket trial demonstrated a median overall survival of up to 15 months in unresectable or metastatic ATC, compared to the historical 3–6 months.
- Guidelines: Neoadjuvant dabrafenib/trametinib is now an NCCN category 2B recommendation for patients with resectable or borderline resectable tumors, enabling some previously inoperable cases to undergo curative resection.
- NTRK Gene Fusions (<5%)
- Agents: Larotrectinib, Entrectinib, Repotrectinib.
- Use: Highly selective TRK inhibitors approved for NTRK fusion–positive solid tumors, including rare cases of ATC. Durable responses and significant tumor shrinkage have been documented in clinical reports.
- RET Gene Fusions (<5%)
- Agents: Pralsetinib, Selpercatinib.
- Evidence: RET-specific inhibitors have shown strong activity in RET fusion–positive thyroid cancers, with reports of clinical benefit in ATC as well.
- Immune Checkpoint Inhibition
- ATC with high tumor mutational burden or PD-L1 expression may respond to PD-1/PD-L1 blockade.
- Agents: Pembrolizumab, Nivolumab.
- Current status: Used alone or in combination with kinase inhibitors, checkpoint inhibitors can achieve disease control in a subset of patients, especially when integrated into multimodal regimens.
- VEGFR-targeted TKIs
- Agents: Lenvatinib, Sorafenib.
- Use: Off-label; sometimes combined with pembrolizumab in ongoing trials.
Prognosis of Anaplastic Thyroid Cancer
- ATC carries an exceptionally poor prognosis:
- responsible for up to 50% of all deaths related to thyroid cancers
- Median survival: 3–6 months with conventional therapy.
- Mortality: Majority of patients dies within a year.
- With molecularly guided therapy: Median survival extended to 7–15 months in selected cohorts; occasional long-term survivors reported.
- Favorable prognostic features in anaplastic thyroid carcinoma include
- younger age (≤60 years),
- absence of nodal or distant metastases,
- small tumor size,
- unilateral involvement,
- lack of local invasion, and
- incidental detection of ATC within a thyroidectomy specimen.
Emerging Directions & Future Perspectives
- Rapid molecular testing (NGS-based) including BRAF, TERT, TP53, NTRK/ALK, PD-L1 is increasingly central to guiding therapy.
- AI and radiomics: Being studied in thyroid cancers for diagnostic and prognostic applications—though specific ATC applications are exploratory
- Multidisciplinary care: Fast-track pathways, expert pathology review, and coordination among surgeons, oncologists, radiologists, pathologists enhance outcomes
Conclusion
Anaplastic thyroid carcinoma remains one of the most formidable malignancies, with an aggressive natural history and dismal prognosis. Yet, the therapeutic landscape has begun to shift.
Key innovations—such as rapid genomic profiling, BRAF/MEK-targeted therapy, and immunotherapy combinations—along with multimodal care strategies, have extended survival and fostered renewed optimism. Moving forward, early diagnosis, tailored molecular therapy, and collaborative multidisciplinary models remain vital for improving patient outcomes.