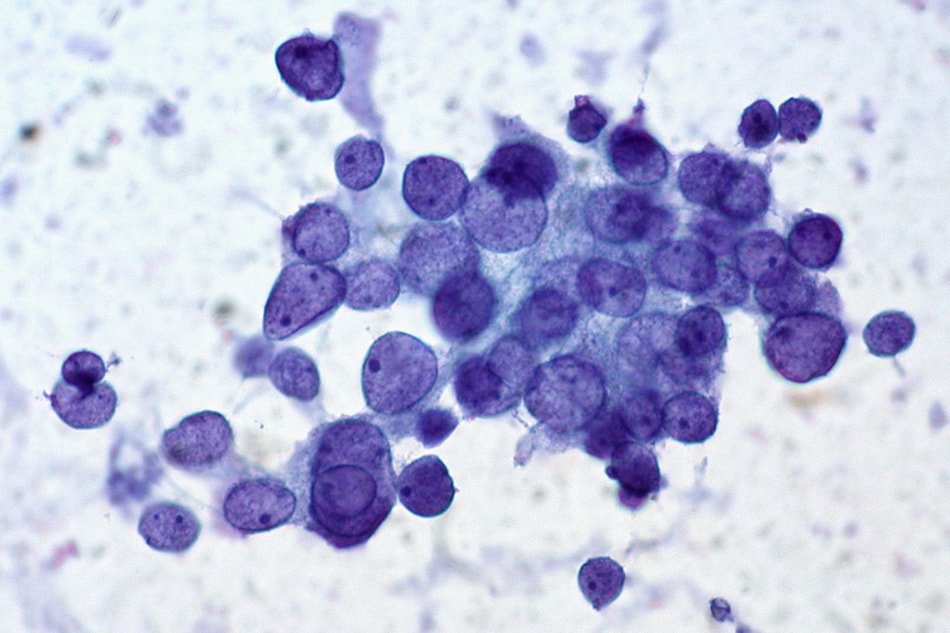
Fine needle aspiration cytology (FNAC) is a corner stone investigation done in the evaluation of thyroid lesion. It is a simple, safe, quick and cost-effective outpatient procedure for diagnosing thyroid patholodies.
FNAC has got a high degree of diagnostic accuracy (85-100%) and a high positive predictive value for malignant diseases (94%). The results are superior when FNAC is performed under ultrasound-guidance (USFNAC).
In this procedure, a small sample of thyroid tissue is removed from the gland with the help of a 24-27G needle under local anesthesia and is looked under a microscope to identify any pathologies.
Need for a universal reporting system / Bethesda System
In order to avoid the nonuniform, ambiguous and confusing terminologies used by cytopathologists for reporting thyroid FNAC throughout the world, the National Cancer Institute (NCI) organized a “Thyroid Fine Needle Aspiration State of the Art and Science Conference” in Bethesda, Maryland in the year 2007.
In this conference, they proposed the Bethesda System for Reporting Thyroid Cytology (TBSRTC) which established a standardized, category-based reporting system for thyroid fine-needle aspiration (FNAC) specimens.
The primary purpose of terminologies used in the Bethesda system is to have a clarity of communication between the cytopathologist and the surgeon, endocrinologist or radiologist. The terminologies should provide clinically relevant information, which should have an implied (or explicit) risk of malignancy on which recommendations for patient management (eg, annual follow-up, repeated FNAC, surgical lobectomy, near-total thyroidectomy) can be based.
Various studies have shown that the Bethesda system for reporting thyroid cytology reduces interobserver variability in reporting thyroid FNACs. TBSRTC also improves communication between the cytopathologist and surgeon by way of indicating cancer risk in each category. In addition, it also provides guidelines for management and allows easy and reliable sharing of data between different laboratories.
2007 Bethesda – 1 system
The 2007 Bethesda system recommends six general diagnostic categories and suggests that each report should begin with a general diagnostic category. Each of the categories has an implied cancer risk (ranging from 0 to 3% for the benign category to nearly 100% for the malignant category) with rational clinical management guidelines.
Category I — Nondiagnostic or unsatisfactory (ND/UNS) : This group involves specimens showing nonspecific features not conclusively diagnostic of a particular entity. These include cyst fluid only, virtually acellular specimens or others like obscuring blood, clotting artifact, etc. In regular practice, this should be ideally limited to no more than 10% of total thyroid FNACs.
Category II — Benign : This category includes benign follicular nodule (colloid nodule, adenomatoid nodule), lymphocytic (Hashimoto’s) thyroiditis and granulomatous (subacute) thyroiditis.
Category III — Atypia of undetermined significance (AUS) or follicular lesion of undetermined significance (FLUS) : In this category, FNAC specimens that do not fit into benign, suspicious or malignant categories are included. This terminology is reserved for specimens containing cells (lymphoid, follicular) with architectural atypia which is not sufficient to be classified as suspicious for a follicular neoplasm (FN) or malignancy and on the other hand atypia is more marked than benign change. The pathologist should specify if it is Hurthle type or Oncocytic type.
Category IV — Follicular neoplasm (FN) or suspicious for a Follicular neoplasm (FN/SFN) : In this category, specimens with significant alteration in the follicular cell architecture, characterized by cell crowding, micro follicles, dispersed isolated cells and scant or absent colloid are included.
Category V — Suspicious for malignancy : This category includes lesions suspicious for papillary carcinoma, medullary carcinoma, other malignancies (eg, lymphoma, metastatic carcinomas), or neoplasm because of total necrosis of lesional cells (e.g., anaplastic carcinoma).
Category VI — Malignant lesion: This category includes specimens with cytomorphologic features which are conclusive for malignancy.
After its introduction in 2007, the Bethesda system got widespread acceptance, especially in the U.S., The American Thyroid Association (ATA) endorsed the system officially in 2015 as part of their revised ATA guidelines and risk stratification. TBSRTC is now the most common classification worldwide for the reporting of thyroid FNAC specimen.
The new advances in the field like Noninvasive Follicular Thyroid Neoplasm with Papillary-Like Nuclear Features (NIFTP), the utility of molecular and IHC markers, and clinical management advancements has necessitated a need for revision of the TBSRTC system. Hence, a second edition for the system was released by the International Cytology Congress, in a symposium held during its meeting in Yokohama, Japan, in 2016.
2017 Bethesda – 2 system for thyroid
Following are the highlights in 2017 revised Bethesda system.
- Every thyroid FNAC report should begin with one of six diagnostic categories, the names of which remain unchanged since they were first introduced:
- nondiagnostic or unsatisfactory
- benign
- atypia of undetermined significance (AUS) or follicular lesion of undetermined significance (FLUS)
- follicular neoplasm or suspicious for a follicular neoplasm
- suspicious for malignancy
- malignant
- There is a choice of two different names for some of the categories. A laboratory should choose the one it prefers and use it exclusively for that category.
- Synonymous terms (e.g., AUS and FLUS) should not be used to denote two distinct interpretations.
- The malignancy risks have been updated based on new data.
- Each category is linked to updated, evidence-based clinical management recommendations.
| Comparison of Bethesda I with Bethesda II (Changes are marked in bold) | ||||
|
| Risk of malignancy | Management option | ||
| Bethesda I | Bethesda II | Bethesda I | Bethesda II | |
| Nondiagnostic or Unsatisfactory | 1-4% | 5-10% | Repeat USG FNAC | Repeat USG FNAC |
| Benign | 0-3% | 0-3% | Clinical and imaging follow-up | Clinical and imaging follow-up |
| Atypia of unknown significance or follicular lesion of undetermined significance. | 5-15% | 10-30% | Repeat FNAC | Repeat FNAC or Molecular studies/diagnostic lobectomy |
| Follicular neoplasm | 20-30% | 25-40% | Surgical lobectomy | Molecular studies/ diagnostic lobectomy |
| Suspicious of malignancy | 60-75% | 50-75% | Lobectomy / Total thyroidectomy | Total thyroidectomy/ lobectomy |
| Malignant | 97-99% | 97-99% | Total thyroidectomy | Total thyroidectomy/ lobectomy |
2023 Update / 3rd Edition of Bethesda
The aim of the recently published third edition of TBSRTC (2023) is to provide a higher degree of granularity to the reporting system by incorporating unified terminology and eliminating duplication in diagnostic nomenclature. It focuses on aligning the Bethesda nomenclature with the recent 2022 World Health Organization Classification of Thyroid Neoplasms, further refining the category-based risk of malignancy estimates. In addition, it introduces cytology-based subcategorization of atypia of undetermined significance (AUS) and includes focused chapters on clinical perspectives, imaging studies, and the use of molecular and other ancillary tests.
Following are the key updates within each diagnostic category follows:
| Diagnostic Category | TBSRTC 2023 Recommendations |
|---|---|
| Nondiagnostic |
|
| Benign |
|
| Atypia of undetermined significance (AUS) |
|
| Follicular neoplasm (FN) and follicular neoplasm–oncocytic follicular neoplasm (FN-OFN) |
|
| Suspicious for malignancy (SFM) |
|
| Malignant |
|
Summary of 2023 Update
| Bethesda System for Reporting Thyroid Cytopathology, third edition, 2023 | |||
|---|---|---|---|
| Diagnostic Category | Examples of Diagnostic Entities | Range of Estimated ROM (%) | Clinical Management Options |
| Nondiagnostic |
| 5–20% | Repeat FNA with ultrasound guidance |
| Benign |
| 2–7% | Clinical and ultrasound follow-up |
| Atypia of undetermined significance (AUS) |
|
| Repeat FNA, molecular testing, diagnostic lobectomy, or surveillance |
| Follicular neoplasm (FN) |
| 23–34% | Molecular testing, diagnostic lobectomy |
| Suspicious for malignancy (SFM) |
| 67–83% | Molecular testing, lobectomy, or total thyroidectomy |
| Malignant |
| 97–100% | Lobectomy or total thyroidectomy |
| FND: follicular nodular disease; AN: adenomatoid nodule; CN: colloid nodule; CLT: chronic lymphocytic (Hashimoto) thyroiditis; PTC: papillary thyroid carcinoma; HGFCDTC: high-grade follicular cell-derived thyroid carcinoma; MTC: medullary thyroid carcinoma; ANTC: anaplastic carcinoma; SCC: squamous cell carcinoma; NHL: non-Hodgkin lymphoma. | |||
References
- Cibas ES, Ali SZ. The 2017 Bethesda System for Reporting Thyroid Cytopathology. Thyroid. 2017 Nov 1;27(11):1341-6.
- Pusztaszeri M, Rossi ED, Auger M, Baloch Z, Bishop J, Bongiovanni M, Chandra A, Cochand-Priollet B, Fadda G, Hirokawa M, Hong S. The Bethesda System for Reporting Thyroid Cytopathology: proposed modifications and updates for the second edition from an international panel. Acta cytologica. 2016;60(5):399-405.
- Renuka IV, Bala GS, Aparna C, Kumari R, Sumalatha K. The Bethesda system for reporting thyroid cytopathology: interpretation and guidelines in surgical treatment. Indian Journal of Otolaryngology and Head & Neck Surgery. 2012 Dec 1;64(4):305-11.
- Cibas ES, Ali SZ. The Bethesda system for reporting thyroid cytopathology. American journal of clinical pathology. 2009 Nov 1;132(5):658-65.
- Baloch, Z.W., Seethala, R.R., Faquin, W.C., Papotti, M.G., Basolo, F., Fadda, G., Randolph, G.W., Hodak, S.P., Nikiforov, Y.E. and Mandel, S.J., 2016. Noninvasive follicular thyroid neoplasm with papillary-like nuclear features (NIFTP): A changing paradigm in thyroid surgical pathology and implications for thyroid cytopathology. Cancer cytopathology, 124(9), pp.616-620.
- Revised thyroid Bethesda System resets malignant risks – Clinical Endocrinology News, August 10, 2017
- Ali SZ, VanderLann PA, eds. The Bethesda System for Reporting Thyroid Cytopathology: Definitions, Criteria, and Explanatory Notes. 3rd ed. Springer Cham; 2023.
- Baloch ZW, Asa SL, Barletta JA, et al. Overview of the 2022 WHO Classification of Thyroid Neoplasms. Endocr Pathol. 2022;33(1):27–63.
- WHO Classification of Tumours Editorial Board. Endocrine and Neuroendocrine Tumours. World Health Organization; 2022. WHO Classification of Tumours; 5th ed., vol. 8. Beta version. https://tumourclassification.iarc.who.int
- Ali SZ, Baloch ZW, Cochand-Priollet B, Schmitt FC, Vielh P, VanderLaan PA. The 2023 Bethesda System for reporting thyroid cytopathology. J Am Soc Cytopathol. 2023; 12(5):319–325.
- Ali SZ, Baloch ZW, Cochand-Priollet B, Schmitt FC, Vielh P, VanderLaan PA. The 2023 Bethesda System for reporting thyroid cytopathology. Thyroid. 2023;33(9):1039–1044.