Pyogenic granuloma (PG), historically a misnomer, refers to a rapidly growing, benign vascular lesion that presents histologically as lobular aggregates of proliferating capillaries. Originally described as “human botryomycosis” by Poncet and Dor in 1897 and later termed “pyogenic granuloma” by Hartzell in 1904, the lesion is neither pyogenic nor granulomatous. The preferred histopathological term is lobular capillary hemangioma (LCH).
In the nasal cavity, PG is rare but increasingly recognized due to improvements in nasal endoscopy. It typically arises from the anterior nasal septum (Little’s area), the turbinates, or less frequently, the maxillary sinus, roof, or floor of the nasal cavity. Common presentations include recurrent epistaxis and nasal obstruction. Its etiology remains multifactorial, with associations to trauma, hormonal influences, infections, and iatrogenic interventions.
Etiopathogenesis of Pyogenic granuloma
The exact pathogenesis of pyogenic granuloma remains unclear. Proposed etiologies include:
- Trauma: Chronic nasal irritation, nose picking, nasal packing, intubation, or foreign bodies.
- Hormonal: Increased estrogen and progesterone during pregnancy; PG is also known as granuloma gravidarum.
- Drugs: Rifampicin has been implicated, although inconsistently.
- Angiogenic Factors: Overexpression of vascular endothelial growth factor (VEGF), pSTAT3, and pATF2 transcription factors have been observed. PG may represent a hyperplastic response to local angiogenic stimuli with imbalance between pro- and anti-angiogenic factors.
- Iatrogenic Causes: Surgical trauma, nasal instrumentation, and piercings.
Clinical Features
Common symptoms of pyogenic granuloma include:
- Unilateral Epistaxis: Most frequent presenting complaint (90-95%)
- Nasal Obstruction: Due to the expanding intranasal mass
- Rhinorrhea: Less frequent
- Other symptoms: Facial pain, hyposmia are also occasionally reported
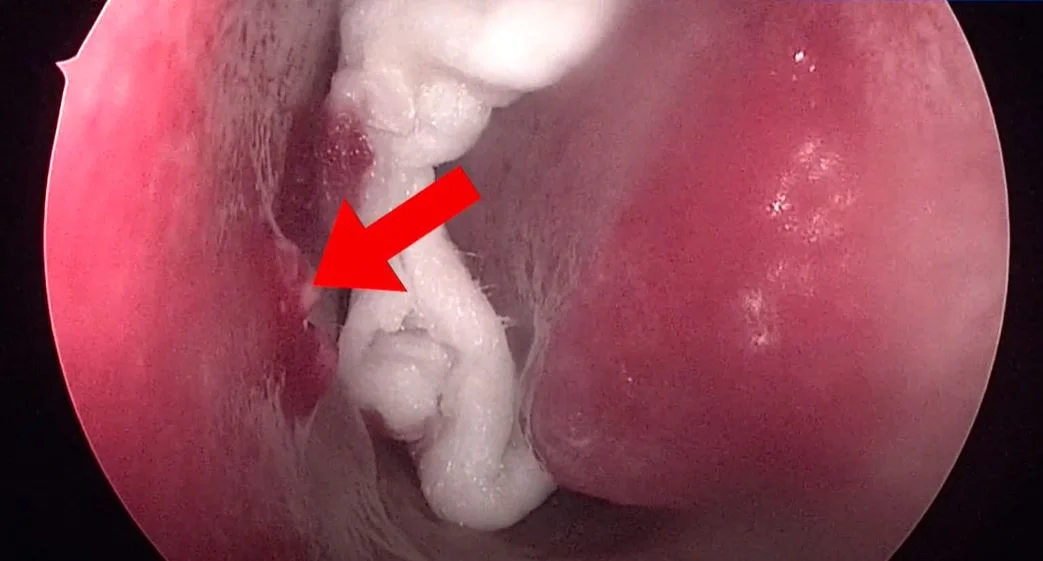
On examination, pyogenic granuloma appears as a red or pink, soft, lobulated, polypoid mass that may be pedunculated or sessile. It may bleed on touch or remain insensitive.
Diagnostic Approach
- Diagnostic Nasal Endoscopy: First-line tool for visualization of lesion location, extent, and origin.
- Imaging: CT and MRI are rarely needed for diagnosis and is reserved for large lesions, suspicion of bone erosion, or differential diagnosis. CT shows well-enhancing masses, while MRI shows T1 hypointensity and T2 hyperintensity.
- Histopathology: Provides definitive diagnosis. Features include capillary lobules surrounded by fibrous stroma and epithelial covering with ulceration.
- Immunohistochemistry: CD31 and CD34 positivity confirm vascular endothelial origin.
Differential Diagnosis of Pyogenic granuloma
- Nasal polyp Hemangiomas (venous, cavernous)
- Arteriovenous malformation
- Granulomatous lesions (e.g., Wegener’s granulomatosis, sarcoidosis)
- Malignant tumors (squamous cell carcinoma, melanoma)
- Inflammatory granulation tissue
Treatment of Nasal pyogenic granuloma
- Endoscopic Surgical Excision: Preferred approach with better visualization and complete removal. Cauterization of the base is done to prevent recurrence. Mucoperichondrial Stripping: Occasionally required.
- Other Modalities Laser Therapy:
- CO2 and Nd:YAG lasers used in selected cases
- Cryotherapy, Electrocautery, Chemical Cautery: Adjunctive or alternative treatments
- Medical Therapy: Experimental use of Rifampicin and Dapsone in resource-limited settings
Endoscopic Surgical Excision of Septal Pyogenic Granuloma
Prognosis and Recurrence
Recurrence is rare with complete excision and cauterization. Lesions typically do not undergo malignant transformation. Spontaneous regression is unusual except in pregnancy-related cases where postpartum involution may occur.
References
- Kulkarni A, Hathiram BT. Pyogenic Granuloma of Nasal Septum. Clin Rhinol Int J. 2011;4(3):163-165.
- Anil Kumar R, Mahesh Babu M, Venkatarajamma PR, Mishra U. Pyogenic Granuloma of Nasal Septum: A Case Report and Review of Literature. Int J Otolaryngol Head Neck Surg. 2014;3(4):190-194.
- Radhakrishnan V, et al. Septal Pyogenic Granuloma: A Continuing Riddle. Int J Otorhinolaryngol Head Neck Surg. 2021;7(12):1947-1949.