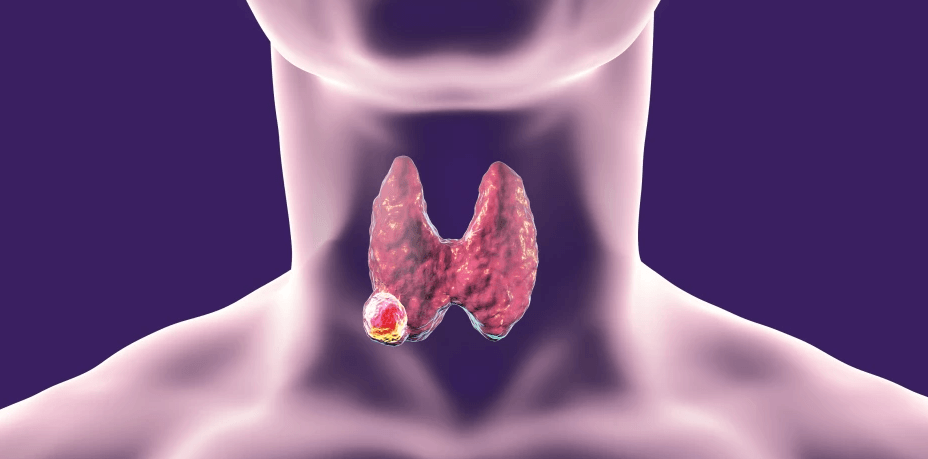
Medullary thyroid carcinoma (MTC) is a neuroendocrine tumor, representing the most uncommon form of thyroid malignancy, comprising nearly 5% of all cases. The cancer arises from the parafollicular C cells, of the thyroid gland, responsible for calcitonin secretion.
MTC presents both as sporadic and hereditary forms. Though the incidence of MTC is less, it accounts for approximately 13% of thyroid cancer-related mortality.
Epidemiology and Etiology
- Approximately 75–90% of MTC cases are sporadic, with the majority presenting as unifocal tumors confined to a single thyroid lobe.
- About half of these sporadic tumors are associated with somatic RET mutations.
- Sporadic tumors that lack RET mutations often have mutations in the RAS pathway.
- These molecular alterations ultimately lead to C-cell hyperplasia and, eventually, carcinoma.
- The remaining 10–25% cases are familial, often bilateral and multifocal, primarily associated with MEN 2A, MEN 2B, or familial non-MEN syndromes.
- MEN 2A (Sipple Syndrome)
- Autosomal dominant with complete penetrance and variable expressivity.
- Triad: Medullary thyroid carcinoma, pheochromocytoma, and hyperparathyroidism.
- MTC presents by the second decade (<35 years) in affected individuals.
- RET proto-oncogene mutations on chromosome 10 (various codons).
- MEN 2B
- Aggressive Medullary thyroid carcinoma with pheochromocytoma, mucosal neuromas, marfanoid habitus, and ganglioneuromas of the gastrointestinal tract.
- Typically due to a single RET mutation at codon 918 (Met918Thr).
- Familial Non-MEN MTC
- RET-positive in ~90% of cases.
- Autosomal dominant inheritance pattern without other endocrine abnormalities.
- MEN 2A (Sipple Syndrome)
Clinical Presentation
- Sporadic MTC
- typically presents during the fifth or sixth decade of life.
- often present similarly to other thyroid cancers, most commonly with a thyroid nodule.
- Familial
- Those associated with MEN can present as early as childhood or the first decade of life, while patients with FMTC usually present in the second or third decade.
- Unlike other types of thyroid cancer, MTC does not exhibit a gender predominance.
- Symptoms caused by local compression or invasion, such as hoarseness, dysphagia, or dyspnea may be present.
- Positive family history.
- Approximately 15% to 50% of patients have clinically evident cervical lymphadenopathy at diagnosis.
- MTC may also be associated with symptoms related to elevated calcitonin levels (eg, diarrhea or flushing), ectopic Cushing syndrome, or positive familial screening.
Diagnostic Workup
- The diagnostic approach is same as evaluating any thyroid nodule. This includes USG neck, Thyroid function tests, along with Fine needle aspiration cytology.
- Other investigations are
- Imaging
- Neck X-ray: Bilateral upper lateral thyroid calcifications.
- Ultrasound Neck: Hypoechoic lesions with microcalcifications, cervical lymphadenopathy.
- Contrast CT Neck, Chest, Abdomen / MRI: Solid masses with coarse or psammomatous calcifications; vascular involvement may necessitate MR angiography.
- MIBG Scintigraphy: Identifies MIBG-avid tumors potentially responsive to MIBG therapy.
- Biochemical Markers
- Serum Calcitonin: Primary tumor marker; elevated in active disease. For patients with calcitonin levels greater than 500 ng/mL, extensive disease on neck ultrasound, or clinical or radiologic evidence of distant metastasis, additional imaging is necessary for comprehensive staging.
- Carcinoembryonic antigen (CEA): Baseline CEA is noted, and it is serially monitored during follow-up for identifying metastatic or recurrent disease.
- Medullary carcinoma patients should be screened for MEN syndromes – Urine VMA, USG Abdomen etc to rule out pheochromacytoma
- Genetic Testing
- Genetic testing should be performed in all cases of MTC to identify germline mutations and other targetable mutations.
- About half of the sporadic tumors are associated with somatic RET mutations, while the remaining cases are linked to mutations in the RAS pathway.
- RET mutation screening is standard for all MTC patients and their families. If RET negative, risk of familial disease is <0.5%. If positive, prophylactic thyroidectomy is advised, following exclusion of pheochromocytoma.
- Histopathology
- Gross Pathology – Gray-white tumor with gritty texture.
- Microscopy
- Common features: hemorrhage, necrosis, fibrosis, and calcifications.
- Spindle-shaped uniform cells in a fibrous stroma.
- Characteristic amyloid deposits, derived from calcitonin, are often observed.
- Imaging
Treatment of Medullary Thyroid Carcinoma
- Staging is based on the AJCC TNM Staging System for Thyroid Cancers
- Requires a multidisciplinary and individualized approach based on factors such as whether the disease is sporadic or hereditary and whether it is resectable or unresectable.
Surgical Treatment
- Surgical intervention is the cornerstone of treatment for MTC.
- Pre-operative evaluation to exclude pheochromocytoma is critical.
- Definitive surgery includes: Total thyroidectomy along with bilateral central compartment (Level VI & VII) clearance including thymectomy.
- Lateral neck dissection (Radical Neck Dissection /Modified Radical Neck Dissection /Selective neck dissection) as needed.
- If MTC is diagnosed post operatively or after incomplete surgery, completion thyroidectomy with appropriate neck dissection is mandatory.
Adjuvant Therapy
- Radioiodine therapy / Radio Iodine Scan: Ineffective due to the parafollicular origin (non-iodine concentrating cells) of the cancer.
- External Beam Radiotherapy: Indicated for gross residual disease or extensive nodal involvement with extracapsular spread. Also used in inoperable cases and to alleviate pain from bone metastases.
Chemotherapy:
- For inoperable cases, systemic therapy options include tyrosine kinase inhibitors (Vandetanib, Cabozantinib), as well as RET-specific inhibitors (Selpercatinib) are considered. PD-1 Inhibitors like Pembrolizumab is considered when no satisfactory alternatives exist.
- No standard regimen; limited efficacy.
- MIBG therapy may be useful for MIBG-avid tumors.
Genetic Counseling and Family Screening
- RET mutation testing is central to identifying hereditary cases. All first-degree relatives should be screened if a familial mutation is identified.
- The presence of C-cell hyperplasia and multiple tumor foci suggests hereditary MTC, even without known family history.
- In familial medullary thyroid carcinoma, the timing of prophylactic thyroidectomy is primarily guided by the specific RET mutation and serum calcitonin levels.
- Early surgical intervention—preferably before the age of 5 years—is recommended for individuals harboring high-risk mutations, such as those at codons 609 and 611.
- In patients with lower-risk RET mutations may be managed with active surveillance, including periodic neck ultrasonography and calcitonin monitoring, with thyroidectomy deferred until there is biochemical or radiological evidence suggestive of MTC progression.
Prognosis
- The prognosis depends on the patient’s age, histologic grade, and surgical resection status.
- Cervical and mediastinal nodal metastasis is observed in nearly 50% of cases.
- Distant metastases to lung, liver, and bone occur in 15–25% of patients.
- Older patients, patients with higher-grade lesions, and those with incomplete surgical resection have a worse prognosis.
- Prognosis is poorer compared to differentiated thyroid cancers, particularly in advanced or hereditary forms.
- The 5-year survival rate for stages I to III is 93% compared to 28% for stage IV.
Surveillance
- Assessment for residual or recurrent MTC should begin with serum calcitonin and CEA measurements approximately three months following surgery.
- If both markers markers are normal limits, follow-up testing is advised every 6 to 12 months.
- When serum calcitonin is elevated, imaging studies are warranted.
- For calcitonin levels below 150 pg/mL, a high-resolution neck ultrasound is typically sufficient.
- When calcitonin exceeds 150 pg/mL, comprehensive imaging—such as contrast-enhanced CT or MRI of the neck, chest, and abdomen, a bone scan, or spinal MRI—should be performed in addition to neck ultrasound.
- Brain MRI is reserved for patients presenting with neurological symptoms suggestive of central nervous system involvement.
- In asymptomatic individuals with persistently elevated tumor markers but no identifiable disease on imaging, close biochemical and clinical surveillance is essential. If residual thyroid tissue is suspected due to incomplete initial surgery, reoperative intervention should be considered when anatomically and clinically feasible.