Lemierre’s syndrome (also known as postanginal septicemia) is a rare, life-threatening complication of oropharyngeal / deep neck space infections (parapharyngeal abscess, retropharyngeal abscess etc..) with significant mortality. It is the septic thrombophlebitis of internal jugular vein in association with and metastatic infections.
The condition was first reported by Andre Lemierre in 1936. In his series of 20 patients, he presented it as a syndrome marked by recent oropharyngeal infection, evident internal jugular (IJV) venous thrombosis through clinical or radiological means, and anaerobic septicemia, primarily attributed to Bacillus funduliformis (now known as Fusobacterium necrophorum). Lemierre termed it as “anaerobic postanginal sepsis” because of the onset of sepsis occurring shortly after the patients had experienced a sore throat.
Clinical features of Lemierre’s syndrome
- Incidence of 3.6 cases per 1 million per year
- Classically affects otherwise young, healthy individuals with 70% of patients between the ages of 16 and 25 years.
- There is a slight male predominance.
- Patient presents with severe unilateral neck pain, features of septicemia, typically developing 4-5 days following an episode of acute pharyngitis / infection of upper aerodigestive tract.
- May also appear secondary to infections including the lungs, middle ear, mastoid, teeth and sinuses.
- Swelling and redness over the angle of the jaw and along the sternocleidomastoid muscle
- Metastatic infections occur in 63%-100% of patients, with lungs being the common site followed by major joints, liver.
- Evidence of pulmonary embolism, spiking fevers, chills, septic arthritis, jaundice/hepatomegaly.
Diagnosis and Evaluation
- High index of suspicion is necessary to diagnose the condition, especially when any of the following are true: pharyngitis that does not resolve in 3 to 5 days; pharyngitis followed by systemic or respiratory symptoms such as fever, chills, rigors or dyspnea; pharyngitis associated with lateral cervical pain and dysphagia; and pharyngitis followed by sepsis or multiple pulmonary abscesses.
- Blood Culture – Fusobacterium necrophorum is the most common organism. One third of patients have a polymicrobial bacteremia, with anaerobic streptococci and other miscellaneous gram-negative anaerobes frequently present.
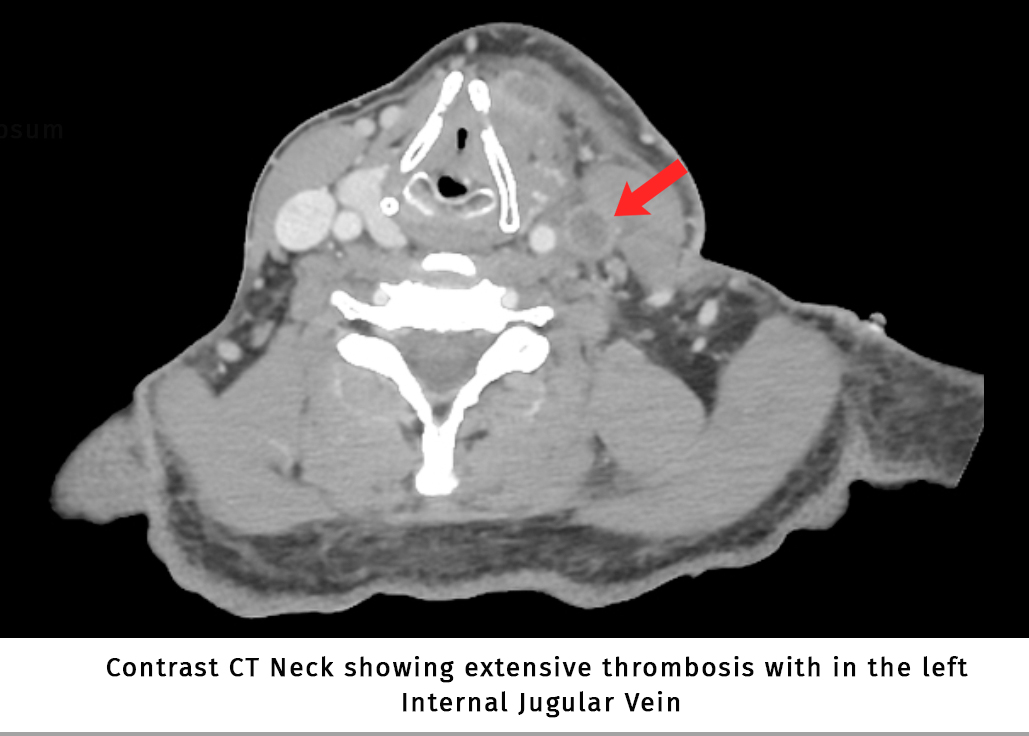
- Skilled imaging with USG shows thrombus in IJV.
- Contrast-enhanced CT is considered the gold standard.
- Chest Xray helps to rule out metastatic lung infections – typically begin as multiple, usually nodular infiltrates that progress rapidly to cavitary lesions and are frequently accompanied by pleural effusions.
- Arthrocentesis if symptoms of septic arthritis.
Treatment of Lemierre’s syndrome
- Prolonged (6 weeks and above) broad spectrum antibiotic with anaerobe coverage is needed.
- Anticoagulation for 3 months if evidence of thrombophlebitis.
- Fibrinolytics can be prescribed if this syndrome is recognized within 4 days of onset.
- Surgical ligation / resection of internal jugular vein is reserved for patients with evidence of septic pulmonary emboli not resolving to medical management.
- Endovascular stenting / superior vena cava filters can also be considered.
Complications
- In the pre-antibiotic era mortality rate was 90%, and in modern era mortality rates ranges from 0%-18%.
- Disseminated intravascular coagulation has been reported in 3%-9% of cases.
- Thrombosis may propagate from the IJV inferiorly into the subclavian vein or superiorly into the cavernous, sigmoid or transverse sinuses.
- Dural venous thrombosis, Meningitis, Cerebral abscess may also complicate up to 3% of cases.
- Carotid aneurysm
- Septic pulmonary emboli