Eagle syndrome, also known as styalgia, stylohyoid syndrome, styloid syndrome, or styloid–carotid artery syndrome, is a rare clinical condition resulting from an elongated or malformed styloid process. This abnormality can lead to compression of nearby nerves, causing orofacial and cervical pain, which is often exacerbated by neck movements.
The first documented case of abnormal mineralization of the styloid ligament complex was reported in 1937 by Dr. Watt Eagle, after whom the syndrome is named. Eagle identified a normal styloid process length as 2.5 to 3.0 cm, with lengths exceeding 3 cm being classified as abnormally elongated.
Anatomy of the Styloid Process
The styloid process extends caudally, medially, and anteriorly toward the maxillo-vertebro-pharyngeal recess, an area containing the carotid arteries, internal jugular vein, and several cranial nerves, including the facial, glossopharyngeal, vagus, and hypoglossal nerves.
Together with the stylohyoid ligament and the lesser horn of the hyoid bone, the styloid process forms the stylohyoid apparatus, which originates embryologically from Reichert’s cartilage of the second branchial arch. The normal length of the styloid process is 2 to 3 cm, with lengths exceeding 3 cm considered elongated.
The styloid process serves as the origin for three muscles—the stylohyoid, styloglossus, and stylopharyngeus—and two ligaments, the stylohyoid and stylomandibular ligaments.
Etiology
The exact etiology of this disease is unknown. Dr. Watt Eagle proposed that surgical trauma, such as tonsillectomy, or local chronic irritation could lead to osteitis, periostitis, or tendonitis of the styloid process and the stylohyoid ligaments. This, in turn, could cause reactive ossifying hyperplasia.
In 1975, Lentini hypothesized that persistent mesenchymal elements, or residues of Reichert’s cartilage, might undergo osseous metaplasia in response to traumatic or stressful events. Epifanio, in 1962, suggested that the ossification of the styloid process might be linked to endocrine disorders in menopausal women, who also exhibit ossification in other body ligaments.
Gokce C et al. (2008) reported that patients with end-stage renal disease, characterized by abnormal calcium, phosphorus, and vitamin D metabolism, displayed heterotopic calcification, which could lead to styloid process elongation and the manifestation of Eagle syndrome.
Lastly, a 2015 retrospective study by Sekerci found a correlation between the presence of an arcuate foramen and an elongated styloid process, based on data from 542 patients using three-dimensional CT scans.
Incidence
- Eagle syndrome is estimated to occur in approximately 4% of the population.
- The condition is more commonly observed in females than males, with a female-to-male ratio of about 2:1.
- Unilateral elongation of the styloid process is more frequently reported than bilateral elongation.
- Clinically, the syndrome is most frequently seen in the third or fourth decades.
Symptoms of Eagle syndrome
Patients with Eagle syndrome may experience dull, intermittent, or persistent pain in areas supplied by the glossopharyngeal and vagus nerves. This pain is often aggravated by swallowing or palpation of the styloid process.
Eagle syndrome can be categorized into two main subtypes:
- Classical (or Eagle) Syndrome: This subtype is typically associated with cranial nerve compression, often occurring after tonsillectomy. Patients may experience pharyngodynia localized in the tonsillar fossa, thought to result from tightened scar tissue moving across the tip of the elongated styloid process during functional movements. Symptoms related to cranial nerve (V, VII, IX, X) compression or irritation may include:
- Facial pain when turning the head
- Dysphagia
- Foreign body sensation in the throat
- Pain when extending the tongue
- Voice changes
- Sensation of hypersalivation
- Tinnitus or otalgia
- Carotid (or Styloid–Carotid Artery) Syndrome: This subtype involves the compression of the internal and/or external carotid arteries, leading to vascular or ischemic symptoms. Pain along the course of the affected artery, believed to be mediated by the sympathetic plexus, is common. Symptoms may include:
- Mechanical compression of the artery
- Visual disturbances
- Syncope or transient ischemic attacks (TIA)
- Carotid dissection (in rare cases)
- Irritation of the sympathetic plexus (carotidynia)
- Eye pain
- Parietal headache
Eagle syndrome can also be classified based on the anatomical characteristics of the styloid process:
- Type I: Elongated and unsegmented styloid process.
- Type II: Styloid process with pseudo-articulated segments.
- Type III: Completely segmented styloid process.
Differential Diagnosis
When evaluating Eagle syndrome, it’s important to consider the following conditions:
- Cervical Arthritis: Arthritis in the cervical spine can cause neck pain and discomfort similar to that of Eagle syndrome.
- Cervical Mass: A mass or lesion in the cervical region may present with symptoms overlapping with those of Eagle syndrome.
- Faulty Dental Prostheses: Issues with dental prostheses can cause localized pain and discomfort that might mimic symptoms of Eagle syndrome.
- Migraine-Type Headaches: Migraines can present with orofacial pain and may be confused with the pain of Eagle syndrome.
- Esophageal Diverticula: Diverticula in the esophagus can cause symptoms such as throat pain or a foreign body sensation.
- Otitis: Infections of the ear can cause pain that may radiate to the throat or jaw.
- Possible Tumors: Tumors in the head and neck region can present with similar symptoms and should be ruled out.
- Salivary Gland Disease: Disorders affecting the salivary glands can cause pain and swelling in the region that might be mistaken for Eagle syndrome.
- Temporal Arteritis: Inflammation of the temporal artery can cause headaches and pain that may overlap with symptoms of Eagle syndrome.
- Trigeminal Neuralgia: This condition causes severe facial pain and should be considered in the differential diagnosis.
Diagnosis of Eagle syndrome
The diagnosis of Eagle syndrome is typically based on the following criteria:
- Clinical Symptoms: The presence of symptoms consistent with the classic form of Eagle syndrome, such as pain in the distribution of the glossopharyngeal and vagus nerves, often aggravated by swallowing or head movements.
- Palpation: Tenderness or pain elicited by palpation of the styloid process tip in the tonsillar fossa. The grading of Eagle syndrome is based on the relationship between the tip of the styloid process and the tonsillar fossa:
- Grade 1: The tip of the styloid process reaches the superior pole of the tonsil.
- Grade 2: The tip of the styloid process reaches the middle of the tonsillar fossa.
- Grade 3: The tip of the styloid process extends to the lower end of the tonsil or enters the base of the tongue
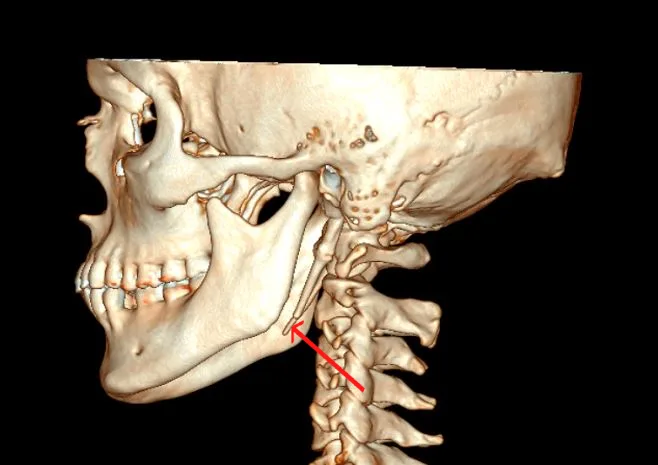
- Imaging Studies: Radiographic evidence, such as X-rays, CT scans, or 3D imaging, showing an elongated styloid process.
- The normal length of the adult styloid is approximately 2.5 cm, while greater than 3 cm is considered elongated. If this criterion is used, almost 4% of the population have an elongated process. However, only a small proportion (4-10%) is symptomatic.
Investigations
The following imaging studies are commonly used to diagnose Eagle syndrome:
- X-ray:
- Towne’s View: Provides a frontal perspective to evaluate the styloid process and its relation to surrounding structures.
- Lateral View: Offers a side perspective to assess the length and orientation of the styloid process.
- Orthopantomogram (OPG): A panoramic dental X-ray that can help visualize the styloid process and its proximity to the jaw.
- CT Scan with 3D Reconstruction: Provides detailed images of the styloid process and surrounding anatomical structures, allowing for precise measurement and assessment of elongation or segmentation.
Treatment of Eagle syndrome
Conservative / Medical Management
- Pharmacological Therapy: Medications such as anti-epileptics, antihistamines, vasodilators, neuroleptics, antidepressants, and tranquilizers may be used as supportive therapy, with Gabapentin (300 mg/day) commonly prescribed. The benefits of these treatments can vary among patients.
- Non-Surgical Treatments:
- Reassurance: Providing emotional and psychological support.
- Nonsteroidal Anti-Inflammatory Medications (NSAIDs): To reduce inflammation and pain.
- Steroid Injections: To alleviate symptoms, typically combined with local anesthetics.
- Stellate Ganglion Block:
- Procedure: A combination of Hydrocortisone (50 mg in 2 ml) and 0.5% Bupivacaine (1 ml) is used for this block.
- Technique: Landmarks include the ear lobe, Frankfurt Horizontal Plane (FHP), and the attachment of the masseter muscle on the ascending ramus. The needle (25-G, 38-mm long) is inserted below the ear lobe, 2 mm distal to the posterior border of the ascending ramus, and 10° posterior to perpendicular at the skin surface. After reaching a depth of 12 mm and aspirating, 0.5 ml of the steroid-local anesthetic combination is injected. The needle is advanced another 6 mm, and the syringe angled anteriorly by 30°, with an additional 1.5 ml of solution deposited at a total depth of 24 mm. A total of 0.5 ml is administered at the stylomandibular ligament insertion, with 1.5 ml around the styloid-stylohyoid apparatus.
- Intraoral Administration: 0.5 ml of the steroid-local anesthetic combination is administered to the region of the lingual nerve using the standard technique for inferior alveolar and lingual nerve blocks in the pterygomandibular space.
Surgical Management
Surgical management is excision of the elongated styloid process, known as styloidectomy.
Intraoral Approaches: Per Oral Trans-tonsillar Styloidectomy: Removal of the styloid process via the oral cavity. A tonsillectomy may be needed.
Extraoral Approaches: External Styloidectomy: Involves an incision outside the oral cavity to remove the elongated styloid process.