Thyroglossal duct cyst (TDC) is a frequent congenital midline anomaly of the neck which usually manifests during the first decade of life. TDC is an epithelial lined tract that connects the tongue to the thyroid gland.
Pathogenesis of thyroglossal cyst
To understand the pathogenesis of thyroglossal cyst, let’s have a look at the embryological development of normal thyroid gland.
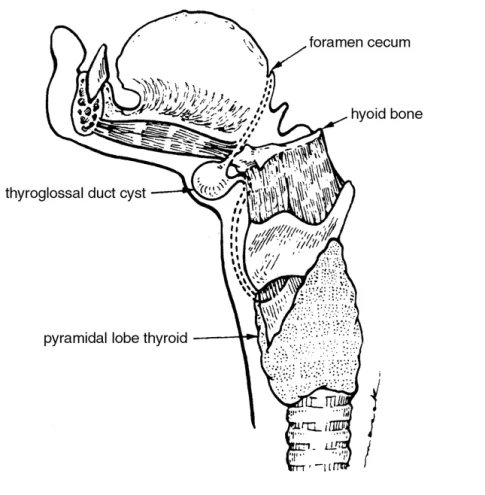
- At around 17th day of gestation, thyroid gland appears as a proliferation of endodermal tissue in floor of primitive pharynx between tuberculum impar and hypobranchial eminence. This site later forms the foramen caecum.
- These proliferated cells of thyroid gland tissue then descends into the mesoderm (the tongue tissue) and then into the hypopharyngeal eminence (which later forms the pharynx) as a cord of cells.
- During this descent, thyroid tissue retains its communication with foramen caecum. This communication is known as thyroglossal duct.
- The gland reaches its final position in neck by 7th week of gestation.
- By around 10th week, the duct starts involuting although the caudal end remains as pyramidal lobe of thyroid.
- The thyroid gland starts functioning by 3rd week of gestation.
- Persistence of the duct can lead to cystic degeneration and formation of thyroglossal cyst.
Path of the duct
As explained above, the duct starts from foramen caecum, passes via the tongue muscle genioglossus, runs in-front / through / behind the hyoid bone to reach the upper border of thyroid cartilage.
Since hyoid bone is formed embryologically at a later stage and is a structure which fuses in midline, the cyst tract gets trapped in its body.
Fate of duct
In most cases, the duct completely atrophies except in its lower part, where it forms thyroid isthmus and pyramidal lobe. The duct can disappears upto hyoid, and the rest forms the Levator Glandulae Thyroidae.
Sites of formation of thyroglossal cyst
The cystic swelling can occur in neck in any part along the line of thyroglossal duct. In 20% of cases, it will be suprahyoid. In 65% cases, most commonly, the cyst is observed in subhyoid location. In 15% cases, it occurs with in body of hyoid and in another 2.1% cases it may be observed at tongue.
Epidemiology
Thyroglossal duct cyst is the most common cystic lesions in neck, accounting for 70% of all congenital neck anomalies, especially in pediatric age group. It is the second most common benign neck mass after lymphadenopathy.
Approximately 7% of the population are thought to have remnants of the thyroglossal duct. The incidence of clinically symptomatic TDC is estimated to be 1 per 1,00,000 – 3,00,000 people. The disease affects both males and females almost equally.
In 30% of cases, it appears before 10 years of age while in 60% it is detected before the age of 20 years.
Clinical features
The disease presentation is often delayed well beyond infancy into early childhood. The tract can lie dormant for years or even decades, until some kind of stimulus leads to cystic dilation.
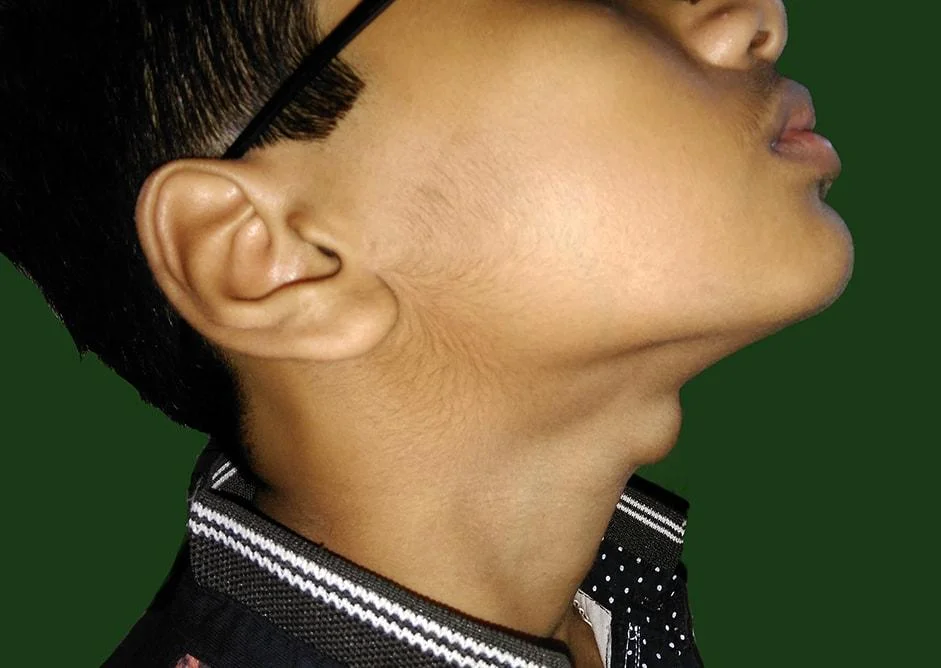
The most common complaint is the neck swelling (83%). Some patients will present with signs of infection (8%), with cutaneous fistula (8%), with neck or throat pain, breathing difficulty and/or dysphagia.
Most often, the swelling will be in midline. But in 10% cases, it may present laterally usually towards left.
On clinical examination, the swelling is a smooth, soft, non-tender, fluctuant, mobile and often transilluminant. The swelling can be moved sideways but not up and down.
Because of attachment to hyoid, the swelling will moves with deglutition as well as protrusion of tongue. A tugging sensation will be felt on protrusion of tongue.
In some cases, the cyst can get infected and the presentation will be as an abscess.
Malignancy, usually papillary carcinoma of thyroid can develop in the cyst.
Differential diagnosis
The differential diagnosis of thyroglossal cyst include other midline neck swellings like
- submental lymph node,
- subhyoid bursa,
- pretracheal lymph nodes,
- dermoid cyst,
- plunging ranula,
- thymic cyst,
- vascular malformations and
- solitary thyroid nodule arising from isthmus of the gland.
Investigations
The diagnosis of thyroglossal cyst is usually a clinical one and the main role of investigations is to look for presence of a normal thyroid. Usually a normal thyroid gland is almost always present, because the thyroglossal duct cyst is the embryologic remnant after the gland has descended.

Thyroid function test
This is to assess the thyroid status of the child. In most of the cases, the child will be euthyroid and no thyroid function tests are required, if the child is clinically euthyroid.
Ultrasound examination of the neck (USG)
USG will show cystic nature of the lesion and will also helps to locate and confirm the position of normal thyroid gland. The absence of sedation and no radiation exposure make this option particularly beneficial for children.
Fine needle aspiration cytology (FNAC)
The diagnosis is usually clinical one and FNAC is unnecessary. This may leads to fistula formation.
Computed tomogram (CT) & Magnetic resonance imaging (MRI) neck
CT and MRI shows midline cystic mass within the infrahyoid strap muscles. CT with contrast shows a well-delineated cystic lesion with capsular enhancement and its relation to the hyoid bone. T2WI MRI is best investigation.
99mTc scan (Scintigraphy)
Scintigraphy will help in confirm the position of thyroid gland and will rule out ectopic gland, but is not routinely performed in children. The investigation is both sensitive and specific for differentiation of an ectopic thyroid from other causes of midline neck masses.
Histopathology of resected specimen
Histopathologically it is a tubulo dermoid type of cyst lined by pseudostratified, ciliated columnar epithelium surrounded by a shell of lymphoid tissue.. The lining epithelium can be cuboidal or squamous epithelium also in some cases too.
The gland will contain transparent thick jelly like fluid, cholesterol crystals and occasionally blood clots. It may contain thyroid tissue.
Treatment
Surgical excision is the treatment of choice in thyroglossal duct cyst. In this operation, excision of cyst and also the full tract up to the foramen caecum is done along with removal of central part of hyoid bone, as the tract passes through it.
Before 1893, the recurrence rate after surgical excision of thyroglossal cyst was more than 50%. In 1893 Schlange proposed excision of cyst along with central portion of hyoid as the treatment for thyroglossal cyst which reduced the recurrence rate by 20%. In 1920, Walter Sistrunk modified this operation and recommended not only taking the central portion of hyoid bone but also carving out a core or tissue one-eighth of an inch in radius from the hyoid bone to foramen caecum. Today Sistrunk operation is considered as the treatment of choice for thyroglossal duct cyst with a 95% cure rate and 95–100% long-term survival. The reported recurrence rate is 0-8% after sistrunk operation.
Surgical steps
- A transverse neck crease incision of approximately 2inches is placed over cyst.
- Subplatysmal flap elevation and cyst with surrounding tissue is dissected up to hyoid bone, avoiding rupture of the cyst.
- Strap muscles are divided.
- The central part of hyoid bone is skeletonized by releasing the strap muscles inferiorly and the geniohyoid and mylohyoid muscles superiorly.
- Hyoid bone is then cut on each side of midline.
- From the superior aspect of the hyoid bone up to the level of the foramen cecum, a core of tissue is then removed as needed, by applying pressure at base of tongue near foramen caecum. The diameter of the core of tissue surrounding the thyroglossal duct is approximately 1cm.
- A drain is inserted near the hyoid bone and the skin is closed over it.
Other surgical methods, though not so popular, are en bloc central neck dissection, suture-guided transhyoid pharyngotomy, and Koempel’s supra-hyoid technique.
Complications
Infection
Infected thyroglossal duct cyst can occur when it is left untreated for a certain amount of time or simply when a thyroglossal duct cyst hasn’t been diagnosed. Soft tissue swelling occurs, along with airway obstruction and trouble swallowing, due to the rapid enlargement of the cyst.
Recurrence
Recurrence is observed mostly when the hyoid bone is not resected. Without removal of hyoid the recurrence rate is 25% and it is less than 5% with removal of hyoid bone. Hence surgery for thyroglossal cyst excision and especially for recurrence should include excision of hyoid and a cuff of tongue base muscle.
Thyroglossal fistula
Thyroglossal fistula develops after infection of thyroglossal cyst which bursts open or after inadequate removal of cyst. The tract is lined by columnar epithelium, discharges mucus and is seat of recurrent inflammation.
Embryologically there exists no communication of TDC with the skin surface of neck and hence congenital thyroglossal fistula never seen.
The hood sign is a characteristic finding in thyroglossal fistula; where the opening of fistula is indrawn and been overlaid by a fold of skin as hood. A radioisotope study and fistulogram can be done prior to sistrunk operation as the treatment.
Carcinoma thyroid
Carcinoma of thyroid is reported in 1-2% cases of thyroglossal cyst.
The etiology of the disease process is not fully understood largely due to the low incidence of the disease. Theories include metastasis, direct extension through the thyroglossal duct, or primary development of carcinoma in the cyst wall or ectopic thyroid tissue.
Primary development of carcinoma in the cyst wall or ectopic thyroid tissue, or the de novo theory, is the leading theory based on current evidence.
Papillary carcinoma is the most commonly reported variant. The other possibilities are follicular variant of papillary carcinoma, squamous cell carcinoma and Hurthle cell carcinoma. The only lesion that has not been found to arise in a thyroglossal duct remnant is medullary carcinoma, which supports the de novo theory, since there are no parafollicular cells in ectopic thyroid.
Most cancers associated with thyroglossal duct cysts are discovered inadvertently at surgery and are identified by pathologic examination. To make the diagnosis of cancer in a thyroglossal duct remnant, it must be distinguished from a cystic lymph node metastasis, and a normal thyroid gland must be present.
Treatment is Sistrunk’s operation and thyroid suppression with thyroxine. An I-131 scan is recommended to prove the thyroid gland is present and to rule out other tumors in the gland. If the thyroid scan is normal, further surgery is contraindicated. If the scan is abnormal, total thyroidectomy is recommended. The scan is repeated after surgery, if differentiated cancer is diagnosed. Post operative thyroid suppression is recommended.
Others
Other complications of surgery are usually minor ones which include hemorrhage, hematoma, superficial surgical site infections, small abscesses around the sutures, seromas and dehiscence of the wound which can be managed on outpatient basis.
References
- Ibrahim, Farid F.; Alnoury, Mohammed K.; Varma, Namrata; Daniel, Sam J. (2015-06-01). “Surgical management outcomes of recurrent thyroglossal duct cyst in children–A systematic review”. International Journal of Pediatric Otorhinolaryngology. 79 (6): 863–867.
- Carter, Yvette; Yeutter, Nicholas; Mazeh, Haggi (2014-09-01). “Thyroglossal duct remnant carcinoma: beyond the Sistrunk procedure”. Surgical Oncology. 23 (3): 161–166.
- Forest V.; Murali R.; Clark JR. (2011). “Thyroglossal duct cyst carcinoma: Case series”. 40 (2): 151–156.
- Al-Thani H, El-Menyar A, Al Sulaiti M, El-Mabrok J, Hajaji K, Elgohary H, Asim M, Taha I, Tabeb A. Presentation, management, and outcome of thyroglossal duct cysts in adult and pediatric populations: a 14-year single center experience. Oman medical journal. 2016 Jul;31(4):276.
- Moorthy SN, Arcot R. Thyroglossal duct cyst—more than just an embryological remnant. Indian Journal of Surgery. 2011 Jan 1;73(1):28-31.
- Wagner G, Medina JE. Excision of thyroglossal duct cyst: the Sistrunk procedure. Operative Techniques in Otolaryngology-Head and Neck Surgery. 2004 Sep 1;15(3):220-3.