Peritonsillar abscess commonly known as Quinsy is localized collections of pus in the peritonsillar space usually occurs as a complication of acute tonsillitis.
Peritonsillar space
- fibrous capsule of palatine tonsils medially and superior constrictor muscle laterally
- anterior and posterior tonsillar pillar contribute to anterior and posterior limits, respectively
- superiorly, this space is related to torus tubarius, while pyriform sinus forms the inferior limit.
- contains loose connective tissue.
Incidence
- Majority of peritonsillar abscess is in young adults between 20 – 40 years.
- Peritonsillar abscess is rare below five years of age
Etiology
- Principal complication of tonsillitis.
- Recurrent attacks of tonsillitis cause obstruction and obliteration of intra tonsillar clefts and the infection spreads to peritonsillar area causing suppuration.
- Smoking and chronic periodontal disease could also cause quinsy.
- Another theory is abscess of Weber’s glands, which are minor salivary glands located in supra tonsillar space.
Symptoms
- Progressive, usually unilateral, sore throat over 3 – 4days.
- Marked cervical lymphadenopathy, leading to neck pain
- Dribbling of saliva, Muffled / Plummy / Hot potato voice.
- Odynophagia (painful swallowing), dysphagia (difficulty in swallowing) for solids and eventually liquids – This results in poor oral hygiene and oral sepsis-causing halitosis (foul breath).
- Severe trismus (inability to open mouth) due to inflammation of the pterygoid muscles.
- Ipsilateral ear ache, fever, lethargy
- If untreated, spontaneous discharge of pus can occur, or it may spread to parapharyngeal and prevertebral space, causing respiratory distress.
- In severe cases, airway compromise and inability to swallow.
Signs
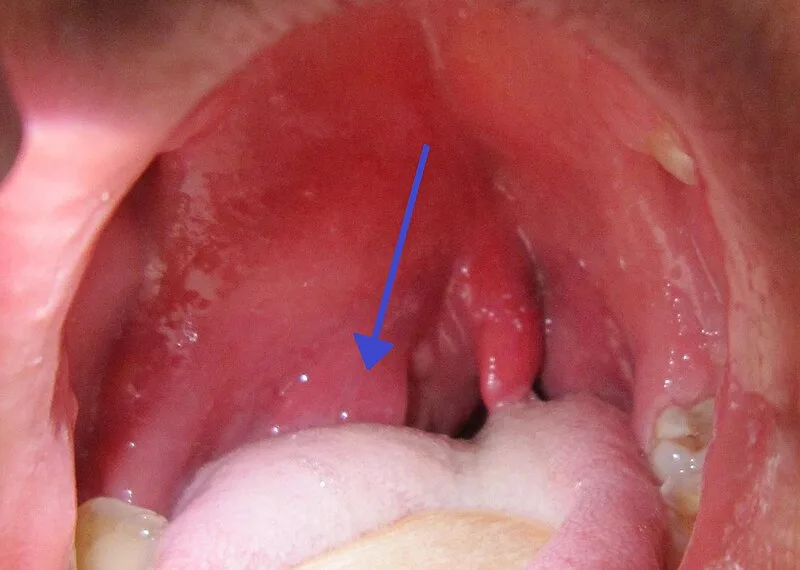
- Predominantly unilateral swelling. (bilateral quinsies are seen in Infectious Mononucleosis – IMN)
- Tonsil pushed downwards and medially
- Blanches on slight pressure
- Uvula edematous and pushed to opposite side.
- Congested pillars, halitosis, trismus, enlarged tender jugulodigastric nodes.
- Cervical lymphadenopathy, usually jugulodigastric lymph nodes.
- Torticollis may be seen as the patient keeps the neck tilted on the affected side.
Differential diagnosis
- Infectious – Peritonsillar cellulitis, Parapharyngeal abscess, Upper third molar abscess, Coexistent IMN.
- Inflammatory pathologies like Kawasaki presenting as peritonsillar abscess
- Vascular – Post traumatic pseudoaneurysm of internal carotid artery
- Benign lesions – Benign lymphoepithelial cyst
- Neoplastic – Carcinoma of tonsils and pillars, tonsillar lymphoma, Rhabdomyosarcoma, Tumors arising from peritonsillar space, Minor salivary gland tumors.
Pathophysiology
- Infection usually starts in the crypta magna of tonsils, from where it spreads beyond the confines of the capsule causing peritonsillitis initially, and peritonsillar abscess later.
- Another proposed mechanism is necrosis and pus formation in the capsular area, which then obstructs the weber glands, which then swell, and the abscess forms.
Microbiology
- Group A Beta Hemolytic Streptococci > Strep. Viridans > S.aureus > H. influenza > Anaerobes.
Investigations
- Not needed in clear cut cases. Mostly the diagnosis is clinical based on
- Non-resolving acute tonsillitis with persistent unilateral tonsillar enlargement
- Unilateral swelling of the peritonsillar area
- A bulge on the unilateral soft palate with anterior displacement of the ipsilateral tonsil
- Investigations are recommended only in atypical cases.
- Needle aspiration of pus
- Often curative
- Provides bacteriology
- Help clarify between peritonsillar abscess and peritonsillar cellulitis.
- Routine screening for IMN is recommended in peritonsillar abscess patients.
- Transoral USG
- Noninvasive method to differentiate PTA from cellulitis.
- Orthopantomogram – In case of coincidental dental disease
- Contrast CT of Neck – In case of suspected complications like spread to parapharynx, retropharynx and mediastinum.
- MRI angiography – In case of suspected vascular anomalies.
- Needle aspiration of pus
- Supportive Investigations
- Complete blood count (CBC)
- Heterophile antibody test (to rule out suspicion of infectious mononucleosis)
- Elevated CRP in patients with suspected sepsis
Treatment of Peritonsillar abscess
- Immediate hospital admission and experienced clinical assessment of airway (can precipitate complete airway obstruction)
- Intravenous (IV) broad spectrum antibiotic with anaerobic coverage + Anti-inflammatory + Antipyretic.
- IV Benzyl penicillin is the antibiotic of choice. Erythromycin is considered in case of penicillin allergy.
- A single dose IV steroid in addition to IV antibiotic reduces throat pain, hospital time, fever and trismus.
- Indications for drainage
- Obvious pointing abscess
- Failure to respond to IV antibiotics
- Evidence of pus in peritonsillar space on imaging.
- Needle aspiration
- Relatively pain free, and is not associated with any significant complication.
- Recurrence rate is 10 – 15%
- Incision & Drainage
- Patient in sitting position to prevent aspiration of pus into the larynx.
- First the oral cavity and throat of the patient is sprayed with 10% topical xylocaine spray to anaesthetize the mucosa.
- A Saint Claire Thompson quinsy forceps, or a guarded 11 blade can be used to prevent the blade from penetrating the tonsillar substance deeply and damaging underlying vital structures like internal carotid artery.
- Site of incision – Is commonly over the point of maximum bulge. It can also be made at the junction between a horizontal imaginary line drawn from the base of the uvula to the anterior pillar and a vertical imaginary line drawn along the anterior pillar. After incision a sinus forceps is introduced for complete drainage.
- Tonsillectomy
- Some surgeons consider tonsillectomy at time of infection – called as hot tonsillectomy
- Avoidance of second admission
- Convalescence from a single episode
- Avoidance of loss to follow up
- Rapid relief of symptoms
- Previously quinsy was considered as an absolute indication for elective interval tonsillectomy – tonsillectomy 6 weeks later after the infection settles.
- Many now consider a second quinsy as reasonable indication for tonsillectomy.
- Abscess recurrence is rare after 40 years. Therefore, elective tonsillectomy is not needed in them.
- Some surgeons consider tonsillectomy at time of infection – called as hot tonsillectomy
Complications of Peritonsillar abscess
- Release of large amount of pus into oropharynx – either spontaneous or surgical – can cause aspiration. This can be avoided by prior aspiration of the pus using a wide bore needle under antibiotic coverage.
- Deep neck space infections and mediastinitis.