Human Immunodeficiency Virus (HIV) associated salivary gland disease is seen in 4-8% of adults and children with HIV, most commonly present as enlarged gland.
The condition is one of the most important HIV-associated oral lesions. The clinical condition is more prevalent in males than in females.
HIV-associated salivary gland disease was first described by Schiodt et al as a recurrent and/or persistent major salivary gland enlargement involving one or both parotid glands with or without xerostomia.
A variety of other lesions can also underlie salivary gland diseases of HIV, these include
- Kaposi’s sarcoma presents as salivary gland enlargement
- Primary or metastatic non-Hodgkin’s lymphoma can be associated with HIV
- Intraglandular lymphadenopathy
- Acute suppurative lymphadenitis
Pathogenesis
- The exact pathology of this disease remains unknown.
- It may be related with HLA-DR5, which is part of more generalized disorder, termed diffuse infiltrated lymphocytosis syndrome (DILS), characterized by CD8+ T-cell infiltration of lungs, salivary glands and lacrimal glands.
Clinical feature of HIV Associated Salivary Gland Disease
- Salivary gland disease is usually a late manifestation of HIV, but can be an early manifestation too.
- Parotids are most commonly affected with profound bilateral, gradual enlargement of the gland with cervical lymphadenopathy.
- Xerostomia / Dry mouth with no other cause such as a side effect of medications.
- There may also be xerophthalmia (dry eyes) and arthralgia (joint pain), mimicking Sjogren’s (SHOW-grins) syndrome.
Differential diagnosis
- Few of the differentials include branchial cysts, salivary duct cysts, reactive lymphadenopathy, traumatic sialocoeles, Sjogren’s syndrome, lymphangiomas, tuberculous abscesses, cystic tumors, malignancies (for example cystadenocarcinoma), as well as those due to Non-Hodgkin’s lymphoma and Kaposi’s sarcoma.
Investigations
- Lab
- Serology – HIV confirmatory blood testing, such as western blot or viral detection.
- Immunology
- Negative anti-Ro (SS-A) and anti-La (SS-B) antibody assay rules out Sjogren’s.
- Patients will have hypergammaglobulinemia.
- Ultra Sonogram (USG) of Parotids
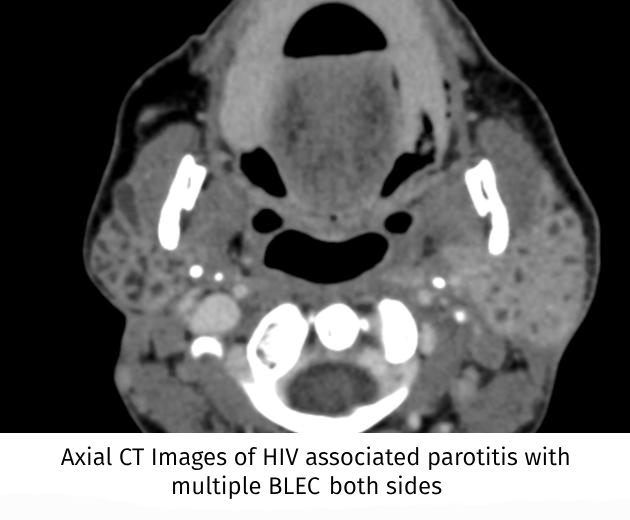
- Multicystic lymphoepithelial cystic lesions (benign lymphoepithelial cysts – BLECs) are characteristic which are thought to be result of hyperplasia of intraglandular lymph nodes.
- BLEC can be defined as the occurrence of single or multiple cysts in the parotid gland lymph nodes.
- BLEC is typically gradual, painless and comprises bilateral parotid swelling with diffuse cervical lymphadenopathy.
- Rarely causes facial palsy and xerostomia
- HIV infection should be ruled out in case of multiple parotid cysts in USG.
- Multicystic lymphoepithelial cystic lesions (benign lymphoepithelial cysts – BLECs) are characteristic which are thought to be result of hyperplasia of intraglandular lymph nodes.
- Fine needle Aspiration Cytology (FNAC)
- FNAC of BLEC reveals a heterogeneous lymphoid population, scattered foamy macrophages and anucleated squamous cells in a proteinaceous background.
- No virus is present in cyst fluid.
- FNAC excludes malignancy – only occurs in less than 1% of patients with HIV-associated cystic lesions
- Histopathology
- Will be similar to Sjogren’s, being dominated by perivascular, periacinar and periductal lymphocytic infiltration, but predominantly by CD8+ T cells
Management of HIV Associated Salivary Gland Disease
- Clinical signs are usually non-progressive and hence therapy is indicated if there is notable cosmetic deformity or xerostomia.
- Anti-Retroviral Therapy (ART) may cause some short-term resolution of swelling.
- External radiation (8-10Gy) can cause transient improvement, although higher doses (24Gy) can cause resolution of disease for at least 24 months – without causing xerostomia.
- Other less practical suggested therapies are repeated aspiration, tetracycline sclerosis or surgical removal of enlarged land.
- BLEC are slowly progressive lesions and any sudden increases in gland size requires prompt investigation due to the risk of lymphomatous transformation.
- Unless neoplasia is suspected, no surgical intervention is needed.