
Drug-induced sleep endoscopy (DISE) has emerged as a valuable diagnostic tool in the evaluation of snoring, sleep-disordered breathing (SDB) offering unique insights into upper airway dynamics during sleep.
Prior to drug-induced sedation, endoscopic evaluation had been reported in natural sleep by Borowiecki in 1978. However, this was a time-consuming process and did not gain much popularity. In 1991, Croft and Pringle first proposed drug-induced sleep endoscopy. Other terms used in the literature include sleep endoscopy, sleep nasendoscopy, somno-endoscopy, somno-scopy, sedated endoscopy, and propofol sleep endoscopy.
Sleep-disordered breathing, encompassing conditions such as obstructive sleep apnea (OSA), hypopnea, and snoring, poses significant health risks and diminishes the quality of life for affected individuals. Traditional diagnostic modalities, such as polysomnography (PSG), offer essential information about sleep architecture but often fall short in pinpointing the specific anatomical sites of airway obstruction.
Drug-Induced Sleep Endoscopy (DISE) involves real-time observation of all pharyngeal and laryngeal upper airway obstructive events during respiratory efforts while maintaining intact protective respiratory reflexes using drug-induced sedation.
Surgery for OSA, once a reserved treatment option for failed conservative measures, is fast becoming one of the first-line options, as well as a salvage option, for appropriately screened patients to choose from. DISE enables surgeons to visualize and understand the dynamic changes occurring in the upper airway during sleep, particularly helping them customize operative procedures to the specific condition of each patient.
Advantages of DISE
- Dynamic Assessment of Airway: DISE allows for a real-time, dynamic evaluation of the upper airway during sleep, providing valuable insights into the specific anatomical and functional changes contributing to airway obstruction.
- Directs an Initial Site-Specific Treatment Plan: By pinpointing the exact location and nature of airway obstruction, DISE facilitates the development of targeted treatment plans, optimizing the effectiveness of interventions.
- Patient-Specific and Site-Specific Therapies: DISE enables a personalized approach to therapy, tailoring interventions based on the individual characteristics and specific site of obstruction identified during the procedure.
- Identifies Causes for CPAP/Primary Treatment Failures: DISE plays a crucial role in uncovering the underlying reasons for the failure of primary treatments such as Continuous Positive Airway Pressure (CPAP), guiding clinicians in adjusting therapeutic strategies accordingly.
- Combines with Split Night PSG and CPAP Titrations: DISE can be seamlessly integrated with other diagnostic methods, such as split-night polysomnography (PSG) and CPAP titrations, providing a comprehensive assessment of sleep-disordered breathing and facilitating streamlined diagnostic and treatment approaches.
- Phenotyping of Patients: DISE contributes to the characterization of patient phenotypes, allowing for a more nuanced understanding of the diverse presentations of sleep-related breathing disorders.
- Identification of Unique Causes for OSA: DISE stands out as a modality capable of identifying specific causes for obstructive sleep apnea (OSA) that may be overlooked by other investigative methods, such as epiglottic collapse and adult laryngomalacia.
- Interventional DISE Predicts Treatment Options and Outcomes: When performed as an interventional procedure, DISE assists in predicting potential treatment options and outcomes, aiding clinicians in making informed decisions about the most suitable therapeutic interventions for individual patients.
Disadvantages of DISE
- Pharmacologically Induced Sleep (Not Natural) and Variable Collapse Sites: DISE involves pharmacologically induced sleep, which may not precisely replicate natural sleep conditions. Additionally, the observed collapse sites may vary during different sleep stages, potentially influencing the accuracy of the assessment.
- Lack of Standardization (Subjectivity): DISE interpretation can be subjective, leading to potential variability in results among different practitioners. The absence of standardized criteria may affect the reliability and reproducibility of the procedure.
- Endoscope Takes Up Upper Airway Space: The presence of the endoscope itself may alter the upper airway anatomy, potentially influencing the dynamics being observed during DISE.
- False Positives: DISE may yield false positives, indicating airway obstructions that may not be clinically significant or may resolve naturally during normal sleep.
Arousal by Mechanical Stimuli and Secretions: Mechanical stimuli and secretions during the endoscopic procedure may lead to arousal, affecting the natural sleep state and potentially influencing the results. - Mucous and Simultaneous Assessment Challenges: Mucous may impede visualization during DISE, and the challenge of simultaneously assessing all levels of the upper airway may limit the comprehensive nature of the evaluation.
- No Reproducible REM Sleep in DISE: DISE may not reliably reproduce rapid eye movement (REM) sleep, limiting its ability to capture specific aspects of sleep-related breathing disorders occurring during this sleep stage. Hence DISE is not helpful in evaluation of REM-related OSA, which can be categorized as REM-predominant and REM-isolated OSA.
- Unwanted Responses from Drugs Used: The drugs used in DISE, such as Midazolam and Propofol, can induce unwanted responses, including central muscle relaxation and central breathing depression, potentially affecting the accuracy of the assessment.
- DISE as a Snapshot of the Night: DISE provides a snapshot of upper airway dynamics during a specific period, but it does not offer information about the entire night’s sleep, potentially limiting its ability to capture variability in sleep patterns.
- Cost of Procedure: The cost associated with DISE may be a limiting factor, affecting its accessibility and utilization as a diagnostic tool.
Indications for DISE
- Surgical planning
- Predicting success in potential mandibular advancement devices (MAD) users and in helping CPAP failures in understanding the reason for failure.
Contraindications for DISE
- ASA (American Society of Anesthesiologists) Score 3 or Above:
- Description: An ASA score of 3 or above indicates patients with moderate to severe systemic disease.
- Rationale: Higher ASA scores are associated with increased procedural risks, and conducting DISE in these individuals may pose a greater threat to their well-being. Therefore, patients with ASA scores of 3 or above are considered contraindicated.
- Severe Obesity:
- Description: Patients with severe obesity, often defined by a high body mass index (BMI), may be at an increased risk for procedural complications.
- Rationale: Due to the higher procedure-associated risks and the potential for less impactful results on treatment decisions in severely obese individuals, DISE may be considered contraindicated in this population.
- Allergy to the Drugs:
- Description: Patients with a known allergy to the drugs commonly used for sedation during DISE (e.g., propofol, midazolam, dexmedetomidine) may be at risk of adverse reactions.
- Rationale: While this contraindication is relatively uncommon, it underscores the importance of thorough pre-procedural assessments, including a detailed history of drug allergies. In cases of drug allergies, alternative sedative agents may be considered, and the procedure can be tailored accordingly.
- Pregnancy:
- Description: Pregnancy is considered a relative contraindication.
- Rationale: While pregnancy is not an absolute contraindication, caution is exercised due to potential concerns about the safety of sedation on the developing fetus. The risks and benefits must be carefully weighed, and alternative diagnostic modalities may be explored.
- Not a Diagnostic Test for OSA; Not a Replacement for PSG:
- Rationale: DISE is not considered a standalone diagnostic test for obstructive sleep apnea (OSA). Instead, it is a complementary tool that provides valuable information about upper airway dynamics. PSG (polysomnography) remains the gold standard for the diagnosis of sleep-related breathing disorders. DISE serves as a supplemental diagnostic and therapeutic planning tool, offering insights into the anatomical basis of airway obstruction.
Technique of Drug Induced Sleep Endoscopy
- Preparation and Monitoring:
- Setting: DISE should be conducted in a setup equipped with basic cardiorespiratory monitoring (pulse oximetry, blood pressure, electrocardiogram, etc.) and essential resuscitation equipment, including an oxygen supply.
- Optional Monitoring Systems: Ideally, the availability of a target-controlled infusion system (TCI) and a Bi-spectral index score (BIS) system for monitoring the depth of sedation is beneficial, though not mandatory.
- Patient Preparation:
- Nil Per Oral: Similar to routine preparation for other general anesthesia procedures, patients should be nil per oral before DISE to prevent regurgitation and aspiration.
- Reduction of Secretions: To minimize secretions, the administration of atropine and other anticholinergics may be considered prior to the procedure.
- Topical Anesthetic: Administer a topical anesthetic to both nostrils a few minutes before the procedure to enhance patient comfort. Usually, 1-2 puffs of 10% lignocaine spray is administered.
- Patient Positioning and Environment:
- Supine Position: The patient should lie in a supine position on the bed, replicating their usual sleeping habits.
- Optimal Environment: Dim the lights and maintain a quiet environment to minimize awakening stimuli.
- Induction of Sleep:
- Drug Options: Commonly used drugs include midazolam, propofol, dexmedetomidine, remifentanil, and ketamine.
- Bolus and TCI Controlled Infusion: Sleep is induced by a bolus of propofol and/or midazolam, followed by a TCI-controlled propofol infusion.
- Ideal Sedation Level: Sedation with a BIS value between 50-70 is recommended. The ideal drug dose varies according to individual susceptibility to sedative effects, with an average dose of 0.06 mg/kg (propofol) body weight.
- Monitoring and Assessment:
- Equivalent to Natural Sleep: Studies suggest that parameters such as critical closing pressure, upper airway muscle responsiveness, apnea-hypopnea index (AHI), and sites of obstruction are equivalent to those observed during N2 and N3 stages of natural sleep.
- Limitation in Reproducing REM Sleep: REM sleep cannot be reliably reproduced with propofol sedation.
- Duration of DISE: DISE typically takes 15–30 minutes, during which N2 sleep can be achieved.
- Endoscopic Examination:
- Flexible Endoscope: Use the thinnest possible fiber endoscope, ideally with a working channel for secretion aspiration.
- Recording System: If available, use a recording system for video and sound to document the examination.
- Observation and Documentation:
- Obstructive Episodes: Observe obstructive episodes during sleep and perform the flexible endoscopic examination after at least two cycles of obstruction and arousal.
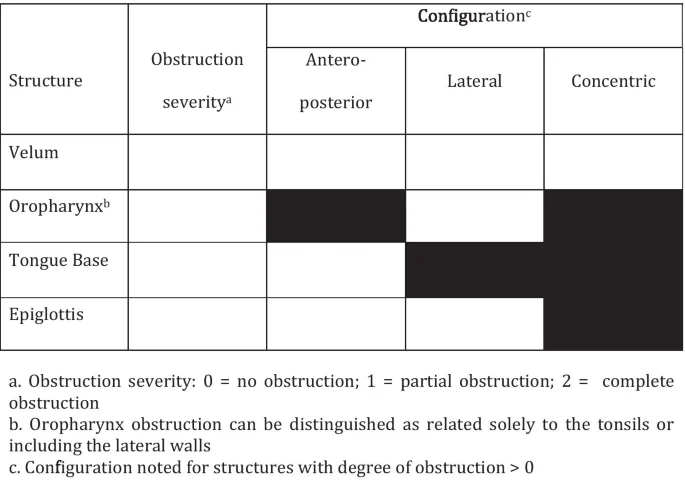
- Documentation: The VOTE classification is a system designed for reporting Drug-Induced Sleep Endoscopy (DISE) findings, specifically focusing on primary structures contributing to upper airway obstruction either alone or in combination: the velum, oropharynx, tongue and epiglottis. This classification system categorizes obstruction sites and characterizes the degree of airway obstruction.
VOTE Classification for DISE
- Velum:
- Location: Scores obstruction at the level of the soft palate, uvula, or lateral pharyngeal wall tissue at the level of the velopharynx.
- Collapse Configuration: Can occur in anteroposterior or concentric configuration, but rarely in lateral configuration.
- Oropharyngeal:
- Components: Includes tonsils and lateral pharyngeal tissues.
- Collapse Configuration: Will have only lateral collapse.
- Tongue Base:
- Collapse Configuration: Anteroposterior collapse.
- Types: Specifies types of tongue base collapse, distinguishing between lymphoid and muscular.
- Epiglottis:
- Collapse Configuration: Only anteroposterior or lateral collapse; no concentric collapse.
- Degree of Airway Narrowing:
- None: No vibration of the involved structure and less than 50% of airway narrowing.
- Partial: Vibration of structures, 50-70% narrowing, reduced airflow.
- Complete: Obstruction, greater than 75% narrowing, and no airflow.
Interventional DISE
Interventional Drug-Induced Sleep Endoscopy (DISE) involves the incorporation of specific maneuvers during the procedure to provide a more nuanced assessment of the upper airway and to simulate therapeutic outcomes. These maneuvers allow clinicians to observe the dynamic changes in the airway under different conditions. Here are the described interventional maneuvers during DISE:
- Chin Lift / Manual Closure of Mouth: This maneuver involves lifting the chin or manually closing the mouth to assess the impact on upper airway dynamics. It helps evaluate the response to changes in head and neck position.
- Jaw Thrust / Esmarch Maneuver: The jaw thrust or Esmarch maneuver involves moving the jaw forward to evaluate its impact on airway patency. This maneuver is particularly useful in assessing the role of the lower jaw in contributing to airway obstruction.
- Using a Nasopharyngeal Airway: Inserting a nasopharyngeal airway can temporarily alleviate upper airway obstruction, providing insights into the dynamic changes in the presence of this intervention. It helps assess the potential effectiveness of using airway devices.
- Turning the Head / Body Laterally: Rotating the head or body laterally helps assess the influence of positional changes on upper airway obstruction. This maneuver is valuable in understanding the impact of sleeping posture on airway dynamics.
- Using / Adjusting Mandibular Advancement Devices (MAD): MADs are devices designed to advance the lower jaw, potentially enlarging the upper airway. During interventional DISE, the use or adjustment of MADs allows for a real-time evaluation of their impact on airway patency.
- CPAP Titration: Continuous Positive Airway Pressure (CPAP) titration involves applying varying levels of positive airway pressure to determine parameters such as Pharyngeal Opening Pressure (POP) and critical closing pressure (pCrit). This helps in understanding the optimal CPAP setting for an individual patient.
These interventional maneuvers during DISE provide clinicians with valuable information about the responsiveness of the upper airway to different interventions. The observations made during these maneuvers aid in tailoring treatment plans and selecting appropriate therapeutic options for individuals with sleep-related breathing disorders.
Negative predictors for surgical success in DISE
- Circumferential collapse at velum
- Lateral collapse at oropharynx after tonsillectomy
- Complete collapse of base of tongue.
- Supraglottic collapse
Other diagnostic tools for assessing dynamic changes in upper airway.
- Respiratory Sound Analysis During Sleep:
- Description: This involves recording and analyzing respiratory sounds, including snoring and airflow patterns, during sleep.
- Application: Respiratory sound analysis provides information on the characteristics of airflow and snoring, aiding in the identification of upper airway obstruction.
- ApneaGraph:
- Description: An ApneaGraph is a portable device that records respiratory parameters, including airflow, respiratory effort, and oxygen saturation during sleep.
- Application: It helps in the detection and quantification of apneas, hypopneas, and other respiratory events, providing insights into upper airway dynamics.
- Acoustic Reflectometry:
- Description: Acoustic reflectometry involves the transmission of sound waves into the airway, and the analysis of reflected signals to assess airway dimensions and collapsibility.
- Application: It provides information on the anatomical features of the upper airway and helps in understanding its dynamic behavior during sleep.
- Cine MRI (Magnetic Resonance Imaging):
- Description: Cine MRI captures a series of images in rapid succession, creating a dynamic video-like sequence of the upper airway during sleep.
- Application: Cine MRI offers a non-invasive way to visualize and analyze upper airway dynamics. However, this is not possible in claustrophobic patients, and it will be difficult to resuscitate patient if something goes wrong.
Recent Advancements
- Advanced Imaging Techniques:
- Three-Dimensional Reconstructions: Researchers have integrated three-dimensional (3D) reconstructions into DISE protocols. This enhancement allows for a more detailed and comprehensive visualization of upper airway anatomy, aiding in the identification of precise sites of obstruction.
- Computational Fluid Dynamics (CFD): The application of computational fluid dynamics to DISE involves simulating airflow within the upper airway. This technique provides insights into the dynamic behavior of airway structures during sleep, contributing to a more in-depth understanding of airflow patterns and potential areas of turbulence.
- Artificial Intelligence (AI) Algorithms:
- Automated Analysis: One of the forefront advancements involves the integration of artificial intelligence algorithms for automated analysis of DISE data. AI holds the potential to streamline the interpretation of endoscopic findings, allowing for faster and more accurate assessments of upper airway dynamics during sleep.
- Pattern Recognition: AI algorithms can be trained to recognize patterns associated with different types of airway obstructions, contributing to a more objective and standardized evaluation of DISE results.
- Quantitative Metrics:
- Objective Scoring Systems: Ongoing research aims to develop objective scoring systems based on quantitative metrics derived from DISE. These metrics may include measures of collapsibility, airway dimensions, and dynamic changes, providing clinicians with more standardized and reproducible data.
- Integration with Other Diagnostic Modalities:
- Multimodal Approaches: Researchers are exploring the integration of DISE with other diagnostic modalities, such as polysomnography (PSG) and imaging studies. This multimodal approach aims to provide a more comprehensive assessment of sleep-related breathing disorders, incorporating both anatomical and physiological data.
- Patient-Centric Considerations:
- Customization of Protocols: Advancements also include efforts to customize DISE protocols based on individual patient characteristics. Tailoring the procedure to account for factors like age, body habitus, and specific sleep-related symptoms contributes to more personalized and clinically relevant assessments.
These recent advancements collectively strive to enhance the diagnostic capabilities of DISE, making it a more precise and efficient tool in the evaluation of sleep-related breathing disorders. The integration of advanced imaging, artificial intelligence, and quantitative metrics holds great promise in elevating the clinical utility of DISE and improving patient outcomes.