
Obstructive Sleep Apnea (OSA) is a common sleep disorder that is characterized by repetitive episodes of partial or complete upper airway obstruction during sleep, resulting in intermittent hypoxia and sleep fragmentation. This results in repetitive cessation of breathing and frequent arousal from sleep.
The condition can lead to significant health complications if left untreated, making early diagnosis and management important.
OSA is a significant public health concern, affecting up to 30% of adults, and has been linked to several serious health consequences, including cardiovascular disease, metabolic dysfunction, and cognitive impairment.
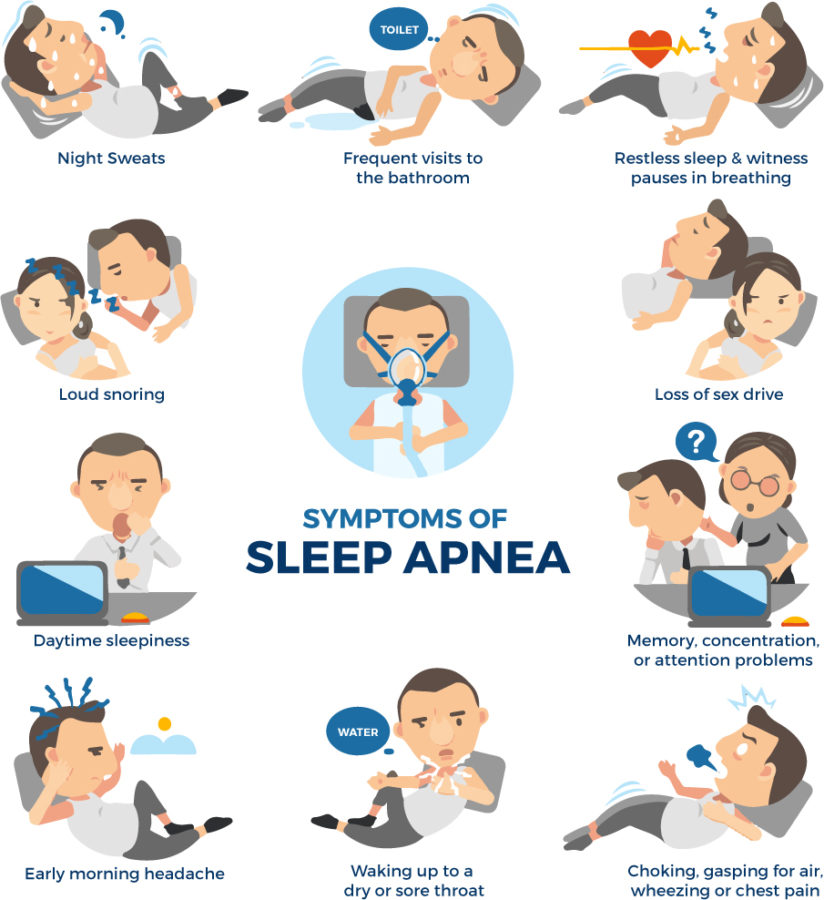
Symptoms of Obstructive Sleep Apnea
The most common symptom of OSA is loud snoring, which is often accompanied by witnessed apneas, choking or gasping sounds, and restless sleep. Patients with OSA may also report
- excessive daytime sleepiness (See the Epworth Sleepiness Scale below),
- waking up with a dry mouth or sore throat,
- waking up with a headache,
- feeling tired or sleepy during the day,
- difficulty concentrating,
- irritability,
- depression, and
- decreased libido.
In severe cases, patients may experience episodes of waking up abruptly during the night feeling short of breath, sweating, and with a racing heart.
Symptoms of obstructive sleep apnea in pediatric patients are hyperactivity in children, worsening depression, poor scholastic performance, bed wetting, teeth grinding and recurrent infections.
Causes
The pathophysiology of OSA is complex and multifactorial. The primary cause of OSA is the collapse of the upper airway during sleep, which is attributed to several anatomical and functional factors, including obesity, craniofacial abnormalities, aging, and hormonal changes.
Obesity is the most significant risk factor for OSA, as excess adipose tissue in the neck and upper airway can narrow the airway and increase airway resistance. In addition, alcohol use, sedative-hypnotic medications, and smoking can exacerbate OSA symptoms by further relaxing upper airway muscles and impairing respiratory drive.
In the pediatric population, adenotonsillar hypertrophy is the most common cause of obstructive sleep apnea.
Risk Factors of Obstructive Sleep Apnea
The risk factors for OSA include obesity, male gender, advanced age, family history of OSA, smoking, alcohol use, and certain medical conditions, such as diabetes, hypertension, and congestive heart failure.
The prevalence of OSA increases with age, with a higher incidence in men than women until menopause when the risk becomes equal. Additionally, OSA is more common in African Americans, Hispanics, and Pacific Islanders, although the reasons for this disparity are not fully understood.
Complications
OSA is associated with several medical comorbidities, including hypertension, cardiovascular disease, stroke, and metabolic dysfunction. The mechanisms linking OSA to these conditions are complex and may involve chronic intermittent hypoxia, sympathetic activation, oxidative stress, and inflammation.
OSA has also been linked to cognitive impairment, including memory deficits, executive dysfunction, and impaired psychomotor performance.
Daytime drowsiness can increase the risk of motor vehicle accidents, occupational injuries, and decreased quality of life. Treatment can help to completely relieve daytime drowsiness.
Diagnosis
The diagnosis of OSA is based on a combination of clinical evaluation, patient history, and objective testing. Patients with suspected OSA should undergo a comprehensive sleep evaluation, including a detailed history and physical examination, overnight polysomnography (PSG), or home sleep apnea testing (HSAT).
PSG is considered the gold standard for diagnosing OSA and involves monitoring several physiological variables, including electroencephalography (EEG), electrooculography (EOG), electromyography (EMG), airflow, oxygen saturation, and snoring. But in most cases for the treatment and diagnosis of OSA, a simple home-based sleep study is enough.
Visit this link to self-test whether you are having Obstructive Sleep Apnea.
Treatment of Obstructive Sleep Apnea
The treatment of OSA aims to alleviate symptoms, improve quality of life, and reduce the risk of complications.
Continuous Positive Airway Pressure (CPAP) therapy
The most effective treatment for OSA is Continuous Positive Airway Pressure (CPAP) therapy, which involves wearing a mask over the nose or mouth during sleep that delivers a continuous stream of air to keep the airway open.
CPAP therapy has been shown to improve sleep quality, reduce daytime sleepiness, and lower blood pressure in patients with OSA.
Lifestyle modifications for obstructive sleep apnea
This includes,
- Weight loss: Losing weight can help reduce the amount of excess fat in the neck area, which can lead to airway constriction and worsening of OSA.
- Avoiding alcohol and sedatives: These substances can relax the muscles in the throat, making it more likely for the airway to collapse during sleep.
- Sleeping in a lateral position: Sleeping on the back can increase the risk of airway obstruction, while sleeping on the side can help keep the airway open.
- Quitting smoking: Smoking can lead to inflammation and narrowing of the airways, which can exacerbate OSA symptoms.
- Regular exercise: Regular exercise can help with weight loss, improve cardiovascular health, and reduce the risk of OSA.
It is important to note that lifestyle modifications may not be enough to treat OSA on their own, but they can be a helpful addition to other treatments, such as CPAP therapy or oral appliances. It is essential to work with a healthcare professional to develop a personalized treatment plan for OSA.
Sleep regularity & Sleep Hygiene
Sleep regularity refers to the consistency of the sleep-wake schedule. This includes both the timing of sleep and the duration of sleep. Consistent sleep patterns help regulate the body’s internal clock, which can improve sleep quality and reduce the risk of sleep disorders.
Sleep hygiene refers to the practices and habits that promote good sleep. This includes creating a sleep-conducive environment, avoiding stimulating activities before bedtime, and practicing relaxation techniques to reduce stress and promote relaxation.
Find out what are the tips for better sleep here:
Oral appliances
These are devices that can be custom fitted by a dentist or orthodontist and are worn in the mouth during sleep to reposition the jaw and tongue to keep the airway open.
Surgery
The role of surgery in OSA is to address the physical obstruction or anatomical abnormalities that are causing the airway to become blocked during sleep. There are several types of surgical procedures that can be performed to treat OSA, including:
- Uvulopalatopharyngoplasty (UPPP): This surgery involves removing excess tissue from the back of the throat, including the uvula and part of the soft palate, to widen the airway and reduce snoring and sleep apnea. This surgery is rarely performed these days, due to high failure rates.
- Expansion sphincter pharyngoplasty (ESP): This modified UPPP procedure involves the removal of excess tissue from the soft palate and the back of the throat, but also includes the addition of a lateral pharyngoplasty, which widens the side walls of the throat. This technique can help to reduce the likelihood of postoperative obstruction and improve outcomes.
- Zeta pharyngoplasty is a surgical procedure that is used to treat obstructive sleep apnea (OSA) by tightening the soft tissues in the back of the throat. It is a relatively new technique that was developed as a modification of the traditional uvulopalatopharyngoplasty (UPPP) procedure.
- Maxillofacial surgery: This type of surgery may be recommended for people with OSA who have a narrow upper jaw or a receding chin. The surgery involves repositioning the jaw to open up the airway.
- Hypoglossal nerve stimulation: This is a newer surgical option that involves implanting a small device that stimulates the hypoglossal nerve, which controls the movement of the tongue and helps keep the airway open during sleep.
It’s important to note that surgery is not always the first-line treatment for OSA and is usually reserved for people who have not had success with other treatments, such as lifestyle changes, continuous positive airway pressure (CPAP), or oral appliances.
Additionally, not all individuals with OSA are candidates for surgery, and the decision to undergo surgery should be made on a case-by-case basis after a thorough evaluation by a sleep specialist.
OSA is a common sleep disorder that can have significant health consequences if left untreated. The diagnosis and management of OSA require a multidisciplinary approach involving sleep medicine specialists, dentists, and other healthcare professionals.
Treatment options for OSA should be individualized based on patient needs and preferences. Treatment adherence is essential to achieve optimal outcomes and reduce the risk of complications. Patients with OSA should also be regularly monitored by a sleep specialist to evaluate treatment effectiveness and adjust treatment as needed.
With appropriate treatment and monitoring, patients with OSA can achieve improved sleep quality, reduced daytime sleepiness, and lower risk of complications.