
Prior to 1990, the mainstay of treatment for oropharyngeal cancers were surgeries. These large, invasive, open approaches like mandibulotomy, tongue pull through (described below), etc were associated with severe compromise in postoperative speech, swallow and airway function of the patient due to violation of pharyngeal mucosa. In addition, surgical management did not avoid the need for adjuvant radiotherapy, hence patients needed multiple treatment modalities.
With the publication of GORTEC trial results, it was shown that side effect profile and complications for surgery were higher, while that of radiation and chemotherapy is more tolerable. These results favored “organ preservation / sparing” with chemo-radiotherapy as the standard treatment for oropharyngeal cancers.
The next major revolution in the treatment of oropharyngeal cancers was the separation of disease into an HPV (Human Papilloma Virus) positive and negative types based on the etiology. 70% of oropharyngeal squamous cell carcinoma (OPSCC) cases were found to be HPV positive. Compared to HPV negative cases, these patients are comparatively younger ones with dramatically improved overall survival.
These younger patients with improved survival were then prone to long-term toxicities from organ-sparing therapies which challenged organ sparing treatment paradigms.
Oncosurgeons started rethinking about surgery for HPV positive oropharyngeal cancers, and by 2003-05 minimally invasive transoral surgical techniques (transoral laser microsurgery & transoral robotic surgery) were evolved and this marks a new era of surgery for OPSCC. These minimally invasive procedures were associated with reduced morbidity and mortality without compromising oncologic outcomes.
Classical Open Surgery in the Treatment of Oropharyngeal Cancers
The classical surgical approaches for oropharyngeal cancers are Transoral (“extended radical tonsillectomy”), Transoral / Transcervical combined (via “delivery” or “pull-through” technique), Transpharyngeal (“suprahyoid / transhyoid pharyngotomy” or “lateral pharyngotomy”), Transmandibular (“composite resection,” “mandibular swing,” and “median labio-mandibulo-glossotomy”). The selection of surgical approaches depends on the size and location of the tumor, whether any concomitant neck dissection needed and based on the plan of reconstruction.
Transoral Approaches
Transoral surgery in the treatment of oropharyngeal cancers is mostly limited to tonsillectomy or extended tonsillectomy. This approach is suitable for Tis / T1 (see the staging of oropharyngeal cancers) superficial or exophytic carcinoma of upper/anterior oropharynx which are readily accessible.
Special instruments like Boyle Davis Gag, FK retractor system may be needed and the dissection can be carried out with laser, scalpel or diathermy. A detailed description of surgical preparation, surgical steps, etc are beyond the scope of this article but can be read from here.
Once resection is carried out, these wounds can be closed either primarily, with local flaps like (facial artery myomucosal flap) or can be left for healing with secondary granulation.
Factors like the presence of trismus, obstructing dentition, excessive soft tissue thickening and height of the mandible, etc limits surgical access to the oropharynx.
The major disadvantages of transoral procedures are limited exposure and risk of injury to the internal carotid artery if resection extends laterally.
Transoral / Transcervical combined approach
This approach is mainly for lesions of the tongue base.
The procedure starts with a neck dissection. A transoral incision is made which extends from ipsilateral anterior pillar to contralateral pillar, crossing midline along the floor of the mouth. The muscle attachment with mandible is released and the tongue is delivered via a pull-through technique. In some cases, the mandibular split is needed for better visualization.
Poor superolateral visualization is the major limitation of this approach. In addition, the procedure is associated with a high risk of injury to the hypoglossal nerve, lingual nerve and artery, and superior laryngeal nerve.
Laterally located oropharyngeal tumors and those involving the glossopharyngeal sulcus or tonsillar region can’t be accessed by this approach.
Transpharyngeal / Suprahyoid pharyngotomy
Suprahyoid pharyngotomy approach is indicated for small tumors of lateral tongue base and pharyngeal wall.
The procedure starts with a neck dissection. The anterior attachment of the digastric muscle is then released. The hyoid bone is identified and skeletonized as in a total laryngectomy. The oropharynx is then entered through vallecula and the tumor is resected.
The procedure is having an excellent functional and cosmetic outcome. It also allows the preservation of lingual arteries and hypoglossal nerve. The incision can be extended laterally and inferiorly along thyroid ala if more exposure is needed, but visualization of superior margins of large tumors is difficult.
Transpharyngeal / Lateral pharyngotomy
This approach allows resection of small tumors of base of the tongue, lateral and posterior pharyngeal wall, tonsil, epiglottis, oropharyngeal wall, and soft palate, without disturbance of the mandible. Tumors with a direct extension of the primary into the neck are contraindications for this approach.
Initial steps are similar to suprahyoid pharyngotomy, the larynx is then retracted to the opposite side and pharynx is entered posterior to thyroid ala on the diseased side.
If needed the incision can be extended across vallecula or can be combined with mandibulotomy. Similar to the transoral / transcervical approach, lateral pharyngotomy is also associated with the chance of injury to the hypoglossal nerve and superior laryngeal nerves.
Transmandibular approach
The procedure is mainly useful for dentulous patients, those with limited mouth opening, posteriorly located tumors.
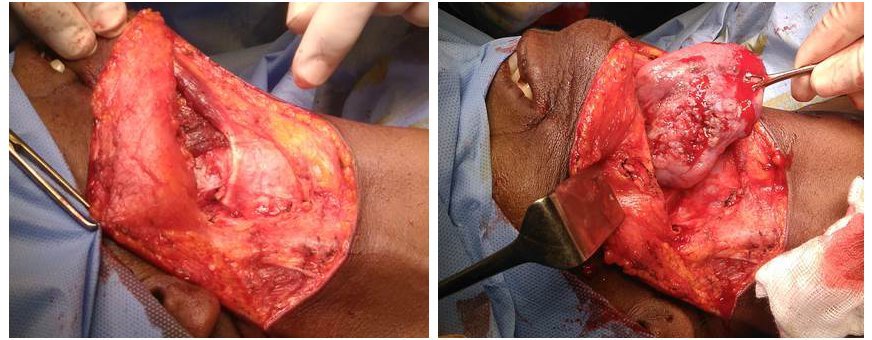
A full-thickness lip splitting incision is given along the mentum into the neck. Via a visor flap approach, the tongue is retracted laterally intraoral incision is made along the gingivobuccal-sulcus and cheek flap is elevated for exposure of the tumor.
Transmandibular / Mandibular swing approach
This approach is indicated for extensive tumors of the lateral tongue base, glossopharyngeal sulcus, tonsil. Mandibular swing approach is also ideal for tumors that don’t involve mandible, tumors involving multiple sites and tumors of parapharyngeal space.
The steps are – lip split incision – mandibular periosteal elevation – mandibular osteotomy – mylohyoid divided – incision along the lateral floor of mouth will be done. Tumor resection will be carried out and a fasciocutaneous flap may be used for reconstruction followed by the closure of floor of mouth and mandibulotomy by mini reconstruction plates.
This approach exposes the entire oropharynx and is the procedure of choice for enbloc resection of the oropharyngeal tumor and neck dissection.
Transmandibular / Median labiomandibular glossectomy
This approach is also known as Trotter’s Operation and was first described in 1929.
The approach is ideal for small midline lesions of the base of tongue and midline posterior pharyngeal wall lesions. The approach also allows access to vallecula or even beyond through a midline suprahyoid epiglottic split, access to the posterior pharyngeal wall and hypopharyngeal walls, etc.
The chance of injury to the hypoglossal nerve and lingual neurovascular bundles are the major drawbacks.
Transmandibular Commando Operation / Composite resection
First described by Ward and Robben in 1951 and this operation is the workhorse for definitive surgical resection of advanced oropharyngeal carcinoma.
COMMANDO is an acronym for COMbined MAndibulectomy and Neck Dissection Operation. The operation is so named because of its extensive nature which comprises en bloc removal of an oral or oropharyngeal tumor, along with mandible, and neck dissection.
The procedure begins with a neck incision which extends from one mastoid tip to another, running parallel to the lower border of the mandible. A lip split incision/raising of visor flap is then done. For neck dissection, the vertical limb of incision is made posteriorly in a lazy-S fashion down the neck. Now wide excision of the lesion (glossectomy) along with a mandibulectomy (hemi/segmental) and enbloc neck dissection is done.
In earlier days the defect was closed with regional myofascial or myocutaneous flaps. Now microvascular free tissue transfer is the standard of care.
Organ Sparing Chemo-Radiotherapy for Oropharyngeal Cancers
As mentioned earlier, with the publication of GORTEC trial results, organ sparing protocols with chemoradiotherapy became the primary treatment modality for oropharyngeal cancers.
A meta-analysis by Parsons et al compared three treatment options for oropharyngeal cancers which include surgery, radiation therapy, or combined treatment. They analyzed 51 retrospective studies and identified 6400 patients with malignancies involving tonsils and/or base of tongue. These patients received either primary surgery with or without post-op adjuvant radiotherapy (S±RT) or primary radiotherapy followed by salvage neck dissection (RT±ND) in residual cases.
They observed that local control, loco-regional control, 5-year overall survival and 5-year disease-free survival were similar in both groups. But the incidence of severe or fatal complications was more (23% Vs 6%) in patients who underwent surgery as the primary modality of treatment. Patients who underwent primary surgery had a poor quality of life due to functional consequences.
The report by Parsons et al concluded that primary radiotherapy followed by salvage neck dissection is ideal for the majority of patients with oropharyngeal squamous cell carcinoma.
A similar study by Pedro et al has also shown that 3-year overall survival and 5-year disease-free interval were not significantly differed for patients who received surgery or radiotherapy. But most patients submitted to primary surgery required adjuvant radiotherapy.
Why not organ sparing protocols?
The RTOG 91-11, RTOG 97-03, and RTOG 99-14 trials have shown that 35% of OPSCC survivors, who received organ preservation chemo-radiotherapy as primary treatment, had severe late toxicity. These include chronic grade 3 or 4 pharyngeal toxicity, gastrostomy dependence beyond 2 years, treatment-related death within 3 years, late-onset treatment-refractory dysphagia affecting 60% of survivors.
In the study by Pedro et al acute grade 3 toxicity was present in 35% cases and late toxicity was observed in 43% cases.
These late-onset adverse effects became a major concern for the newer group of HPV positive patients with dramatically improved overall survival. HPV positive patients are surviving to suffer the long-term toxicities from organ-sparing therapy.
These observations questioned the role of organ preservation in OPSCC and slowly minimally invasive surgical options like transoral laser microsurgery or transoral robotic surgeries came into the picture.
Minimally Invasive Transoral Surgery in the Treatment of Oropharyngeal Cancers
The minimally invasive transoral surgeries for treatment of OPSCC are Transoral Laser Micro Surgery (TLM, Steiner in 1980) and Transoral Robotic Surgery (TORS, McLeod and Melder in 2005).
These surgical options are ideal for T1/T2, N0/1/2a/2b oropharyngeal lesions.
Patients with trismus, involvement of carotid vessels, prevertebral fascia, mandible, with distant metastasis, those who definitely need chemoradiotherapy despite surgical treatment, extensive soft palate involvement, extensive disease into the nasopharynx, with disease extension along the lateral pharyngeal wall, base tongue lesions crossing midline are not ideal for TLM/TORS.
Transoral laser microsurgery (TLM) was popularized by Steiner in 1980.
Studies have shown that control rates of TLM are comparable to classical open surgical treatment and nonsurgical organ preservation treatments. In additional TLM was found to have better functional outcomes compared to chemo-radiotherapy. Only 3-6% of patients remained gastrostomy dependent.
McLeod and Melder were the first to use Robotic surgery in oropharynx for the excision of a vallecular cyst, in 2015.
Park et al have done a systematic review and meta-analysis on the safety and effectiveness of “transoral robotic surgery versus open surgery“. They analyzed 9 retrospective papers with data of 574 patients and observed that the 3-year disease-free interval was higher in TORS than open surgery. Other important observations are – TORS patients had a low risk for free flap reconstruction need, lower feeding tube dependency rate. Time of decannulation (removal of tracheostomy tube) was less in TORS by 6.7 days, time to oral diet was shorter in TORS by 2.2 days and length of hospital stay was shorter by 1.09 days.
In 2016, Morisod B et al did a similar systemic review on the survival of patients treated with “transoral surgery versus radiotherapy“. Their analysis was based on 729 patients in the RT group versus 276 in the TOS group with similar quality of studies in both groups. The results suggest equivalent efficacy of both treatments in terms of disease control for early-stage oropharyngeal squamous cell carcinoma.
Hutcheson et al did a systemic analysis of “functional outcomes after TORS” for oropharyngeal cancer. They analyzed 12 papers, 441 patients who underwent TORS with or without adjuvant therapy. Feeding tube dependence, swallow examination findings, speech ratings, velopharyngeal insufficiency, pneumonia, and oral intake measures were the parameters they analyzed. They observed better swallowing and other functional outcomes with TORS than radiotherapy.
The literature on minimally invasive surgeries is scarce and all the above-mentioned analysis was based on retrospective studies. As of now, no randomized prospective trials exist regarding the role of TORS in oropharyngeal cancers.
Currently, three prospective randomized trials on TORS versus radiotherapy are currently ongoing, these are ECOG 3311, EORTC 1420 and ORATOR trial. Of this, the report of ORATOR trial got published recently. The early results from other trials are expected in 2021.
Ongoing Prospective Trials in Oropharyngeal Cancers
The ORATOR trial (Oropharynx: Radiotherapy Versus Trans-Oral Robotic Surgery) is a phase II prospective trial which studies swallowing outcome of oropharyngeal squamous cell carcinoma patients treated with TORS or radiotherapy. The study was initiated in June 2012, with primary endpoints as quality-of-life outcomes at the end of 1, 3, 5 years and secondary endpoints including overall survival, progression-free survival, toxicity.
The early reports of ORATOR trial published included 68 patients, 34 per group with a median follow-up of 25 months show an unexpected outcome – patients treated with radiotherapy showed a superior swallowing related quality of life scores at 1 year after treatment, although the difference did not represent a clinically meaningful change.
A short follow-up period and a small patient population are the drawbacks of the ORATOR trial. To overcome these limitations, a larger follow-up trial, ORATOR2, is now underway to evaluate the quality of life and survival rates between the two approaches in human papillomavirus (HPV)-associated oropharyngeal cancers.
The ECOG 3311 is a randomized phase II prospective trial involving lateralized, resectable T1-T2 and N1-N2b oropharyngeal squamous cell carcinoma, who undergo TORS with neck dissection, followed by randomized low-Dose or standard-dose risk-based adjuvant therapy. The study was initiated in August 2013 and interim results are awaited.
EORTC 1420 is a similar phase III trial assessing the “best of” radiotherapy compared to the “best of” surgery (trans-oral surgery (TOS)) in patients with T1-T2, N0-N1 oropharyngeal, supraglottic carcinoma and with T1, N0 hypopharyngeal carcinoma. The study was initiated on November 2017, with the primary outcome as patients swallowing. Similar to ECOG 3311, interim reports are awaited for EORTC 1420 also.
Can Surgery Prevent Occurrence of Oropharyngeal Cancers?
Studies based on Swedish and Danish cancer registries found that tonsillectomy significantly reduced the risk of developing tonsillar carcinoma. Based on the Danish registry, from 1977 to 2012, the incidence of tonsillectomies significantly decreased, whereas the incidence of oropharyngeal carcinoma significantly increased. They observed that a remote history of tonsillectomy reduces the risk of diagnosis with tonsil carcinoma.
Contrary to the above, data from the North Carolina Central Cancer Registry shown that prior tonsillectomy was associated with a two-fold increase in the risk of base-of- tongue carcinoma.
But at present, there is a theoretical role of prophylactic surgery in oropharyngeal cancers, but current literature does not warrant prophylactic surgery for oropharyngeal squamous cell carcinoma.
Conclusions
Early-stage oropharyngeal squamous cell carcinoma is currently treated with primary surgery or primary radiotherapy, both with similar control and survival rates. Discussion between the two treatment options is all about toxicities and quality of life. Minimally invasive techniques like TLM / TORS is an ideal surgical option in early OPSCC.
Until randomized trials clarify the benefit of TORS or reduced-dose radiation over conventional treatments the discussion between surgery vs. chemoradiotherapy is still open.
References
- Holsinger, F. C., Laccourreye, O., & Weber, R. S. (2005). Surgical approaches for cancer of the oropharynx. Operative Techniques in Otolaryngology-Head and Neck Surgery, 16(1), 40–48.
- Parsons JT, Mendenhall WM, Stringer SP, et al. Squamous cell carcinoma of the oropharynx: surgery, radiation therapy, or both. Cancer 2002;94(11):2967–80.
- C. Pedro, B. Mira, P. Silva, E. Netto, R. Pocinho, A. Mota, M. Labareda, M. Magalhães, S.Esteves, F. Santos, Surgery vs. primary radiotherapy in early-stage oropharyngeal cancer, Clinical & Translational Radiation Oncology (2017)
- Canis M, Martin A, Kron M, et al. Results of transoral laser microsurgery in 102 patients with squamous cell carcinoma of the tonsil. Eur Arch Otorhinolaryngal. 2013;270:2299–306.
- Canis M, Ihler F, Wolff HA, et al. Oncologic and functional results after transoral laser microsurgery of tongue base carcinoma. Eur Arch Otorhinolaryngal. 2013; 270:1075–1083.
- Haughey BH, Hinni ML, Salassa JR, et al. Transoral laser microsurgery as primary treatment for advanced-stage oropharyngeal cancer: A United States multicenter study.Head Neck. 2011; 33:1683–1694.
- Park DA, Lee MJ, Kim S-H, Lee SH, Comparative safety and effectiveness of transoral robotic surgery versus open surgery for oropharyngeal cancer: A systematic review and meta-analysis, European Journal of Surgical Oncology (2019)
- Morisod B, Simon C. Meta-analysis on survival of patients treated with transoral surgery versus radiotherapy for early-stage squamous cell carcinoma of the oropharynx. Head Neck.2016; 38:E2143–E2150.
- Hutcheson KA, Holsinger FC, Kupferman ME, et al. Functional outcomes after TORS for oropharyngeal cancer: A systematic review. Eur Arch Otorhinolaryngal. 2015; 272:463–471.
- Nichols AC, Theurer J, Prisman E, Read N, Berthelet E, Tran E, Fung K, de Almeida JR, Bayley A, Goldstein DP, Hier M. Radiotherapy versus transoral robotic surgery and neck dissection for oropharyngeal squamous cell carcinoma (ORATOR): an open-label, phase 2, randomised trial. The Lancet Oncology. 2019 Aug 12.