The thyroid gland is a butterfly-shaped gland located at the front of the neck. The job of the thyroid gland is to produce thyroid hormones. Thyroid hormone also helps the brain, heart, muscles, and other organs in the body function as they should. Apart from this hormone, the thyroid gland also produces a hormone called calcitonin which controls the calcium level in the body.
There are many diseases that affect the thyroid gland. Hypothyroidism is the most common form of thyroid disease caused by insufficient production of thyroid hormone. This disease is more common in women than men. In contrast, hyperthyroidism is a medical condition caused by excessive production of thyroid hormone.
Diseases caused by inflammation in the thyroid gland are also known as thyroiditis.
Apart from the above, there is also the possibility of various nodules / lumps in the thyroid gland. If there is only one nodule it is called Solitary Thyroid Nodule and if there are more than one nodule, it is called Multi Nodular Goiter (MNG). More than 90 percent of these tumors are non-cancerous. Less than 5 to 10 percent of tumors are likely to be cancerous.
When is thyroid surgery needed?
Hypothyroidism, hyperthyroidism and thyroiditis can be treated with medicine.
Hypothyroidism is treated with thyroid hormone in pill form. Most hypothyroid patients will need to continue this pill for life.
Although hyperthyroidism can be treated with medication, some patients may require surgery and possibly radioactive iodine therapy to achieve complete relief.
For thyroid nodules, surgery becomes necessary when tumors are confirmed or suspected to be cancerous. However, in cases of non-cancerous nodules, factors such as their size and associated complications (such as swallowing difficulties, voice changes, visual impairments, rapid growth, or concurrent hyperthyroidism) are evaluated to determine the need for surgery.
How many types of thyroid surgery are there?
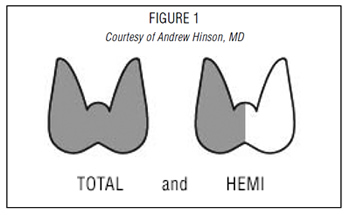
Surgery to remove the entire thyroid gland is called Total Thyroidectomy.
Surgery to remove only one side of the thyroid gland is called hemithyroidectomy. This operation is also known as thyroid lobectomy.
During surgery for thyroid cancer, a neck dissection may sometimes be necessary to remove the neck lymph nodes along with the removal of the gland.
Before thyroid surgery
Prior to thyroid surgery, it’s crucial to evaluate the thyroid gland’s function. This involves conducting blood tests to verify that levels of T3, T4, TSH, and other relevant markers are within normal ranges.
Furthermore, to gain insight into the gland’s structure and assess the risk of cancer, the doctor typically advises ultrasound scanning (USG) and guided fine needle aspiration cytology (FNAC). In certain instances, CT scans and MRI scans may be recommended.
Additionally, any other medical conditions that could complicate surgery or anesthesia administration, such as hypertension, diabetes, or cardiovascular, pulmonary, or renal disorders, should be managed effectively.
How is thyroid surgery performed?
Thyroid surgery is conducted under general anesthesia.
The removal of the thyroid gland is achieved through a small incision in the front of the neck. Alternatively, endoscopic surgery may be employed, accessing the thyroid through the mouth or armpit to minimize visible scarring.
Usually, patients require a hospital stay lasting from one to three to four days.
Following the procedure, a temporary drain is inserted into the neck to facilitate wound drainage. This drain is typically removed within one to three to four days post-surgery.
For the first two weeks following surgery, it’s advisable to avoid heavy exertion. Activities like vigorous sports, swimming, and those involving weight-bearing should be postponed for at least ten days to two weeks. However, there are typically no restrictions on engaging in other daily activities during this time.
What are the complications of thyroid surgery?
In experienced hands, thyroid surgery is generally very safe. Complications in such situations are uncommon. However, some of the most serious risks of thyroid surgery include:
- The recurrent laryngeal nerve plays a crucial role in controlling the vocal cords for speech. Positioned behind the thyroid gland, it is vulnerable to injury during thyroid surgery, which can lead to speech impairment. Thankfully, such impairment is usually temporary. Surgeons take great care to protect this nerve, utilizing nerve monitors during the procedure to detect and prevent damage. However, if both nerves are damaged, there is a risk of respiratory failure.
- Adjacent to the thyroid gland is the parathyroid gland, which regulates calcium levels in the body. These are four small glands about the size of a pea. During surgery, the parathyroid gland is located and protected from damage. However, in most cases, it is normal for this gland to become temporarily inactive. If this happens, calcium tablets and injections may be needed for a few days. This is a temporary problem in most patients. It will change completely after a few days. In rare scenarios, the parathyroid gland is removed unknowingly. If so, calcium tablets should be taken for life.
- Scar mark in the neck – This chance of scar can be avoided in Endoscopic Thyroid Surgery.
- Numbness of the skin on the neck
- Other complications associated with surgery include, in rare cases, wound infection and intra-operative/post-operative bleeding requiring blood transfusion.
Surgical complications are more common in cancer patients, patients undergoing revision thyroid surgery, and patients with very large tumors. Before surgery, patients should understand the reasons for the operation, alternative methods of treatment, risks and benefits of the operation from the doctor.
Although there may be some temporary complications with thyroid surgery, a good percentage of patients make a full recovery in a short period of time.
Whom should you consult for your thyroid surgery?
It is advisable to consult a thyroid surgeon who has special training in thyroid surgery and performs thyroid surgery regularly. Complication rates of thyroid surgery are low when performed by a surgeon who performs many thyroid operations each year.
What should be done to heal the scar?
Scars from surgery usually heal within 12 to 18 months. The most important things to keep in mind for scar reduction are timing, sun protection, and massage.
- Timing: You need to be patient as scars usually heal naturally within 12-18 months.
- Sunscreen: It is very important to protect all wounds from direct sunlight. Sunburn scars can remain red and plump for a long time, perhaps even permanently. It is advisable to use sunscreen on all scars, especially fresh ones. A sunscreen containing zinc oxide or titanium dioxide is best.
- Massage: A gentle massage will help flatten the scars. You can use things like vitamin E oil, cocoa butter, and skin cream to lubricate the skin while massaging. However, none of these moisturizers have been proven to improve scarring. The pressure from the massage itself helps the wound to flatten out without causing scarring. Massage can be started two weeks after the operation. Remember to massage daily for at least 2 months. Along the entire length of the wound, rub with your fingertips in a circular motion, applying steady pressure. It may be painful at first. So do it slowly in the beginning and gradually increase the amount of pressure.
Will hormone pills be needed after surgery?
Patients who have undergone total thyroidectomy are typically required to take thyroid hormone pills for the remainder of their lives.
Research indicates that individuals who have had a hemithyroidectomy may not require thyroid hormone supplementation initially. However, over time, many of these patients may eventually need to start taking thyroid hormone pills.
Can I live a normal life after surgery?
Of course. After the first two weeks are over, you can usually do anything you were able to do before surgery.
When to seek emergency care after Thyroid Surgery?
Although some slight swelling or discoloration of the wound is normal, sudden pain accompanied by oozing, swelling, difficulty breathing or swallowing should prompt immediate medical attention.
Some patients experience numbness around the mouth or in the fingertips/fingers/hands. This is a sign of low calcium levels in the blood. If you experience any of these symptoms, you should contact your doctor immediately.