In the world of medicine, some recoveries are more than just physical—they’re personal, emotional, and transformational. Today, I would like to share the story of a young teacher, whose life took an unexpected turn after a routine surgery, and how a small intervention gave her more than just her voice—it gave her purpose back.
The Silent Complication: Vocal Cord Palsy After Thyroidectomy
Thyroid surgery, particularly thyroidectomy, is a common and generally safe procedure performed for conditions like goiter, thyroid nodules, or cancer. However, one of the known—though rare—complications of thyroidectomy is the injury to the recurrent laryngeal nerve, which supplies the vocal cords.
In experienced surgical hands, the risk of permanent vocal cord palsy is generally low—estimated at 0.5% to 2%, and even lower when intraoperative nerve monitoring is used. Still, when it does occur, its impact can be profound, especially for professionals like teachers, singers, or public speakers.
Understanding Vocal Cord Palsy
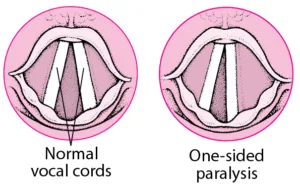
There are two types of vocal cord palsy:
- Unilateral Vocal Cord Palsy – affects one vocal cord
- Bilateral Vocal Cord Palsy – affects both vocal cords
In unilateral palsy, the voice becomes breathy, weak, and often effortful. Patients may experience:
- Difficulty projecting voice
- Vocal fatigue
- Breathlessness while speaking
- Coughing or choking while swallowing liquids
In bilateral palsy, breathing becomes the main concern, sometimes requiring emergency airway intervention, though voice quality may be less affected.
Her Story: When the Classroom Fell Silent
“When I spoke, no one could hear me. When I tried to teach, I could barely be understood. I didn’t know if I could return to the classroom.”
— 32-year-old schoolteacher, post-thyroidectomy
This 32-year-old dedicated schoolteacher underwent thyroid surgery elsewhere for a benign thyroid condition. The surgery went well, but days later, she noticed something was wrong: her voice was hoarse and breathy. Over the next few weeks, it failed to recover.
A laryngoscopic evaluation confirmed our suspicion—left unilateral vocal cord palsy.
For a teacher, the voice isn’t just a tool—it’s the very heart of their profession. Her confidence took a blow. She began doubting if she could return to teaching at all.
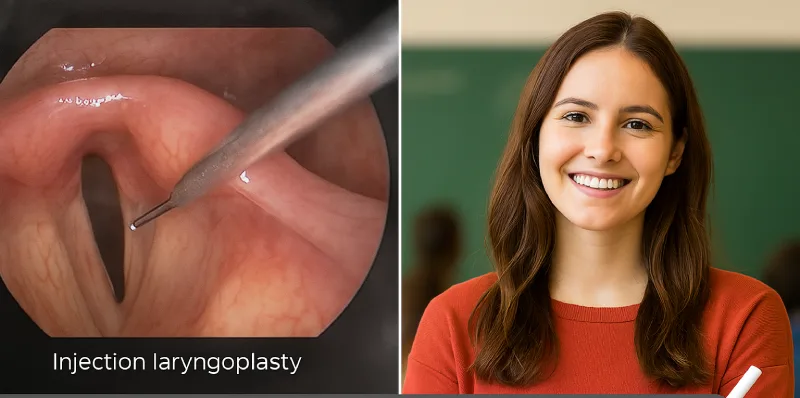
The Turning Point: Injection Laryngoplasty
After assessing the paralysis and allowing time for possible spontaneous nerve recovery, we offered her injection laryngoplasty, a minimally invasive procedure that can immediately improve voice quality.
In this procedure:
- A biocompatible material (like hyaluronic acid, collagen, or fat) is injected into the paralyzed vocal cord – this can be done as an opd procedure or under general anesthesia as a day care procedure.
- This medializes the cord—moving it toward the midline—allowing the opposite, functioning cord to make better contact.
- The result is improved glottic closure, leading to a stronger, clearer, and more natural voice.
In her case, the improvement was dramatic. Her breathy whisper turned into a confident, audible voice. The smile that followed spoke volumes.
Back Where She Belongs
Today, she’s back in her classroom. Teaching. Engaging. Laughing. Living.
She recently told us, “It wasn’t just a procedure. It was a lifeline. You gave me my voice, and my life, back.”
The Takeaway: Why Early Recognition and Treatment Matter
Voice changes after thyroid surgery should never be ignored. If hoarseness persists beyond two weeks, it’s essential to see an ENT specialist. Early diagnosis and intervention—like injection laryngoplasty—can drastically improve quality of life and avoid long-term disability.
This story is a reminder of the delicate balance between anatomy and identity. A tiny nerve, barely the width of a thread, can change a life. And a few drops of injected gel can restore it.
To every surgeon, ENT, and speech therapist—your skill restores more than just function. You restore voices, identities, and dreams.