
Allergic rhinitis, commonly called hay fever, is a condition where body’s immune system overreacts to particles in the air, known as allergens, causing bothersome symptoms that can affect daily life.
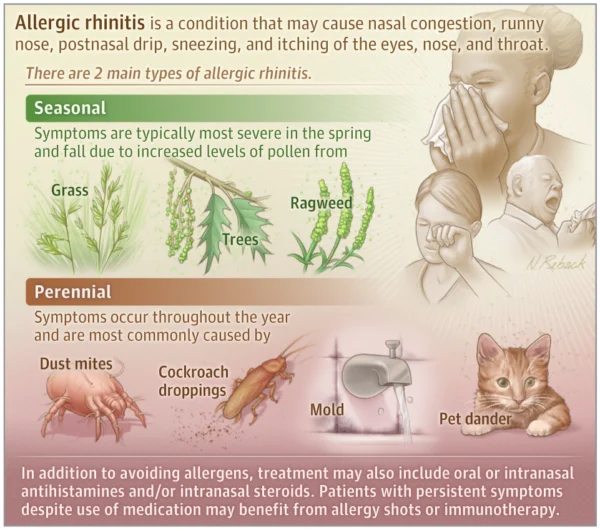
Approximately 50 million Americans and one in 20 Indian’s are affected by this, leading to symptoms such as nasal congestion, sneezing, a runny nose, postnasal drip, and itching in the eyes, nose, and throat.
This is a patient information article explaining the types, causes, and available treatments for allergic rhinitis to better understand and manage this condition.
What Causes Allergic Rhinitis?
Allergic rhinitis is triggered by inhaling allergens, which can be found both outdoors and indoors. When allergens enter the nasal passages, the immune system releases chemicals, including histamines, to counteract the allergens. This immune response is what causes the typical symptoms of allergic rhinitis.
The two primary types of allergic rhinitis are:
- Seasonal: Symptoms are usually more severe during specific seasons, primarily spring and fall, due to high levels of tree, grass, or ragweed pollen. Geographic location can also influence which types of pollen are prevalent, affecting symptom timing.
- Perennial: This type affects people year-round and is often triggered by indoor allergens like dust mites, pet dander, mold, or cockroach droppings.
Who is at Risk?
You may be at increased risk if you have:
- Asthma or eczema: These conditions, along with allergic rhinitis, are common in people with an allergic predisposition, known as atopy.
- Family history: Those with a family history of allergies, asthma, or eczema have a higher likelihood of developing allergic rhinitis.
- Additional conditions: It is often associated with sinusitis, conjunctivitis, ear infections, chronic cough, headaches, and even sleep disturbances like sleep apnea, all of which can further impact quality of life. Sometimes, the allergic symptoms may worse during pregnancy.
Recognizing the Symptoms
Symptoms are similar to a common cold but are triggered by allergens rather than viruses. Key symptoms include:
- Persistent sneezing
- Runny or congested nose
- Itchy, watery eyes
- Itchy throat or inner ear
- Postnasal drip
For some, symptoms can be so severe that they interfere with sleep, concentration, and daily activities.
Diagnosis and Allergy Testing
Diagnosing allergic rhinitis is generally based on medical history and reported symptoms. For persistent or severe symptoms, allergists may conduct tests to identify specific allergens:
- Skin Prick Testing: This is the most common and involves placing small amounts of allergens on the skin and pricking the surface. A reaction, such as a red, raised spot, indicates an allergy to that substance.
- Intradermal Testing: If a skin prick test does not yield clear results, small amounts of allergens may be injected into the skin to test for reactions.
- IgE Blood Testing: Measuring levels of specific IgE antibodies in the blood can also help confirm allergies to various triggers like pollen, pet dander, mold, and dust mites.
Treatment Options for Allergic Rhinitis
Managing allergic rhinitis often requires a combination of lifestyle changes and medications:
- Avoiding Allergens:
- Outdoor allergens: Close windows during high pollen seasons, use air conditioning, and check pollen forecasts to avoid high-pollen days.
- Indoor allergens: Use dust mite-resistant covers, clean bedding frequently in hot water, and keep pets out of the bedroom. High-efficiency particulate air (HEPA) filters in bedrooms and other frequently used rooms can help reduce exposure to airborne allergens.
- Pest control: Exterminate or reduce exposure to pests like cockroaches and rodents.
- Medications:
- Oral Antihistamines: Over-the-counter options like fexofenadine, cetirizine, loratadine, and desloratadine can relieve mild symptoms.
- Intranasal Antihistamines: These sprays (such as azelastine or olopatadine) provide targeted relief for nasal symptoms.
- Intranasal Corticosteroids: Nasal sprays like fluticasone, triamcinolone, budesonide, or mometasone can reduce inflammation in the nasal passages and are often the most effective treatment for moderate to severe symptoms.
- Combination Therapy: For persistent symptoms, combining intranasal antihistamines and corticosteroids can improve effectiveness.
- Nasal Washes (Saline Irrigation):
- Saline nasal rinses or nasal washes can help flush out allergens, reduce congestion, and relieve nasal irritation. Available over the counter, these solutions are effective for both seasonal and perennial allergic rhinitis. Using a neti pot, nasal spray, or rinse bottle can improve symptoms when used consistently, especially before using other nasal sprays.
- Immunotherapy (Allergy Shots or Sublingual Tablets):
- Immunotherapy may be recommended when lifestyle adjustments and medications do not adequately control symptoms. This treatment gradually exposes the body to increasing amounts of an allergen, which helps reduce the immune response over time.
- Subcutaneous Immunotherapy (SCIT): Administered as injections, this therapy is conducted in a medical setting to monitor for reactions.
- Sublingual Immunotherapy (SLIT): This involves placing tablets under the tongue and can often be done at home, offering an alternative to injections.
- Monoclonal Antibodies:
- Newer treatments, such as monoclonal antibodies like omalizumab, are used in cases where allergic rhinitis is severe or doesn’t respond well to other treatments. These drugs work by blocking specific immune responses that lead to allergy symptoms and are typically considered when standard treatments are insufficient.
Living with Allergic Rhinitis
Proper management of allergic rhinitis can significantly improve quality of life. Maintaining a clean environment, using medications as prescribed, and considering immunotherapy, when necessary, can minimize the impact of allergic rhinitis on daily activities.
Reference
- Voelker R. What Is Allergic Rhinitis? JAMA. Published online October 24, 2024. doi:10.1001/jama.2024.14237