![Thyroidectomy © By n.raveender [CC-BY-SA-3.0] via Wikimedia Commons](https://drsanu.com/wp-content/uploads/2019/02/728_large.jpg.webp)
Hyperthyroidism is a clinical condition where the thyroid gland is overactive and produces excess thyroid hormone. The most common causes of hyperthyroidism are Graves’ disease (autoimmune process), toxic nodular goiter and toxic adenoma.
Hyperthyroidism affects approximately 2% of women and 0.2% of men with an estimated annual lifetime risk of 2-5%. The reported incidence of hyperthyroidism has increased annually over the last 20 years, probably as a result of increasing awareness and use of thyroid hormone tests.
It exerts a major influence on the circulatory system with cardiovascular symptoms and signs being prominent. Atrial fibrillation is the most significant manifestation of hyperthyroidism, is reported in 5% to 15% of those who have it.
Hyperthyroidism is also related to a procoagulant state and vascular dysfunction leading to a condition like venous thromboembolism. Increasing evidence suggests that mortality, especially from circulatory disease, is also increased in hyperthyroidism.
Currently, three main treatment options are available for hyperthyroidism, each of them having their own pros and cons. These include antithyroid medications (like Methimazole, Propylthiouracil), radioactive iodine (RAI) or thyroidectomy (surgical removal of thyroid glands).
Mostly, the choice of treatment is influenced by institutional and regional practice patterns, as well as individual patient factors and preferences.
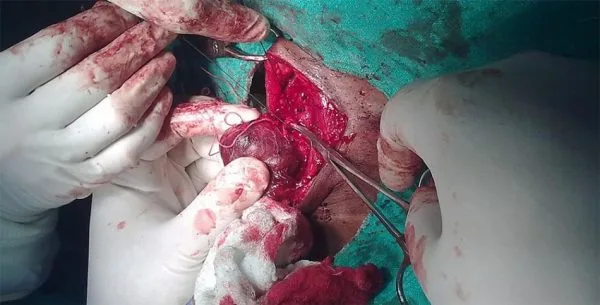
Among the available treatment options, RAI and thyroidectomy are considered as the definitive treatment options because of permanent destruction or removal of the thyroid gland, associated with very low relapse rates.
Antithyroid drugs are associated with a slight risk of cutaneous side-effects, agranulocytosis or hepatic injury, and carry a high risk of relapse into hyperthyroidism once treatment is discontinued.
Less risk of cardiovascular mortality after surgery
Recently, Giesecke P et al. from Department of Clinical Sciences, Danderyd Hospital, Karolinska Institute, Stockholm, Sweden published their study on long term cardiovascular mortality risk after surgery versus radioiodine treatment for hyperthyroidism, using the national Swedish registry, which collects demographic and medical information for the entire country population. Their study can be summarized as follows
- Between 1976 and 2000, a total of 10,250 patients received radioactive iodine therapy, as registered in Stockholm Radioiodine Cohort.
- 742 patients underwent thyroidectomy, as registered in the Swedish National Patient Register.
- Mean follow-up period of 16-22 years.
- Patients were then uniquely matched to the National Patient Register to find comorbid diagnoses.
- The cause of death was obtained from death certificates.
- Women represented 85% of the patients in both groups.
- Patients treated with RAI therapy were older as compared to patients treated with surgery (average age 64 vs. 47 years) and had more baseline medical problems, including heart diseases, such as myocardial infarction and atrial fibrillation, stroke, hypertension, diabetes, and cancer.
- Patients in the surgery group had a higher percentage of thyroid-associated eye disease as compared to the radioactive iodine therapy group (13.2% vs. 8.5%).
- After adjusting the difference in the patients’ age and comorbid conditions, it was observed that surgery group had a lower risk of all-cause mortality and cardiovascular mortality, especially due to heart disease as compared to RAI therapy group during long-term follow-up.
- However, a gender subgroup analysis revealed that only men and not women had a higher risk of death after RAI therapy when compared to thyroid surgery.
- The risk of death due to cancer or other causes was similar for the two treatment groups.
- An increased risk of malignancy following radioactive iodine treatment was not observed in the current study.
Based on their results, the authors made the following conclusions to their study
Surgery for hyperthyroidism was associated with a lower risk of all-cause and cardiovascular death as compared to radioactive iodine therapy during long-term follow-up, particularly in men.
This was the first study reporting a difference in the long-term outcome of the two treatment modalities (radioactive iodine or thyroidectomy) for hyperthyroidism, especially related to cardiovascular diseases.
The limitation of the study was.
- Retrospective design is a major limitation.
- Only 7% of patients with hyperthyroidism were treated surgically – clear selection bias in favor of RAI with the youngest and healthiest patients was selected for thyroidectomy.
- it failed to include information and did not adjust the analysis for the patient’s’ thyroid status after the RAI therapy and surgery, including relapse data since it is known that persistent hyperthyroidism by itself is associated with an increased all-cause and cardiovascular mortality.
What’s other studies saying?
The first of this type of study, examining long-term effects of different treatments for hyperthyroidism, was performed at the Mayo Clinic in 1982, the researchers found no difference in mortality among RAI or surgery groups. Another study from the US in 1988, conducted by Goldman and co-workers observed a slightly increased risk of cardiovascular death in patients treated with RAI compared with surgery or antithyroid drugs. But these two studies were exclusively done in women only.
Previous registry studies from Great Britain and Finland showed an increase in all-cause and cardiovascular mortality in patients treated with radioactive iodine when compared to the general population. Metso et al in their study observed an increased incidence of cerebrovascular and cancer mortality in patients treated with RAI and emphasized the need for long-term vigilance on patients treated with RAI.
Kautbally et al from Belgium in their study of total thyroidectomy vs RAI concluded, total thyroidectomy as more efficient than RAI to induce a rapid and permanent correction of hyperthyroidism.
Conclusions
Currently, radioactive iodine therapy is the preferred definitive therapy for Graves’ hyperthyroidism in the US. However, recent studies have concluded that in patients with Graves’ disease, radioiodine and surgery were equally effective in terms of relapse prevention, but antithyroid drugs were less effective.
Results of these studies are showing that clinical practice trends may be shifting away from radioactive iodine in favor of long-term antithyroid drugs.
Thyroidectomy remains underutilized for treatment of hyperthyroidism both in the United States and worldwide. This study (despite the limitations) and many other cohorts suggest that some patients (particularly men) may have improved long-term outcomes with surgery.
References
- Dekkers OM, Horváth-Puhó E, Cannegieter SC, Vandenbroucke JP, Sørensen HT, Jørgensen JO. Acute cardiovascular events and all-cause mortality in patients with hyperthyroidism: a population-based cohort study. European journal of endocrinology. 2017 Jan 1;176(1):1-9.
- Giesecke P, Frykman V, Wallin G, Lönn S, Discacciati A, Törring O, Rosenqvist M. Allâ€cause and cardiovascular mortality risk after surgery versus radioiodine treatment for hyperthyroidism. British Journal of Surgery. 2018 Feb;105(3):279-86.
- Hoffman DA, McConahey WM, Diamond EL, Kurland LT. Mortality in women treated for hyperthyroidism. Am J Epidemiol 1982; 115: 243–254.
- Goldman MB, Maloof F, Monson RR, Aschengrau A, Cooper DS, Ridgway EC. Radioactive iodine therapy and breast cancer. A follow-up study of hyperthyroid women. Am J Epidemiol 1988; 127: 969–980.
- Franklyn JA, Maisonneuve P, Sheppard MC, Betteridge J, Boyle P 1998 Mortality after the treatment of hyperthyroidism with radioactive iodine. N Engl J Med 338:712–718.
- Metso S, Jaatinen P, Huhtala H, Auvinen A, Oksala H, Salmi J 2007 Increased cardiovascular and cancer mortality after radioiodine treatment for hyperthyroidism. J Clin Endocrinol Metab 92:2190–2196. Epub Mar 20.
- Kautbally, S., Alexopoulou, O., Daumerie, C., Jamar, F., Mourad, M. and Maiter, D., 2012. Greater efficacy of total thyroidectomy versus radioiodine therapy on hyperthyroidism and thyroid-stimulating immunoglobulin levels in patients with Graves’ disease previously treated with antithyroid drugs. European thyroid journal, 1(2), pp.122-128.
- Sundaresh V, Brito JP,Wang Z, Prokop LJ, Stan MN, Murad MH et al. Comparative effectiveness of therapies for Graves’ hyperthyroidism: a systematic review and network meta-analysis. J Clin Endocrinol Metab 2013; 98: 3671–3677.