The field of otolaryngology (ENT) often presents unique challenges, but few are as intriguing and complex as the phenomenon of migratory foreign bodies in the upper aerodigestive tract. Recently, our team had the privilege of publishing our observations and findings on this topic in the Journal of Laryngology and Otology (JLO), shedding light on these rare but significant clinical scenarios.
Understanding Migratory Foreign Bodies
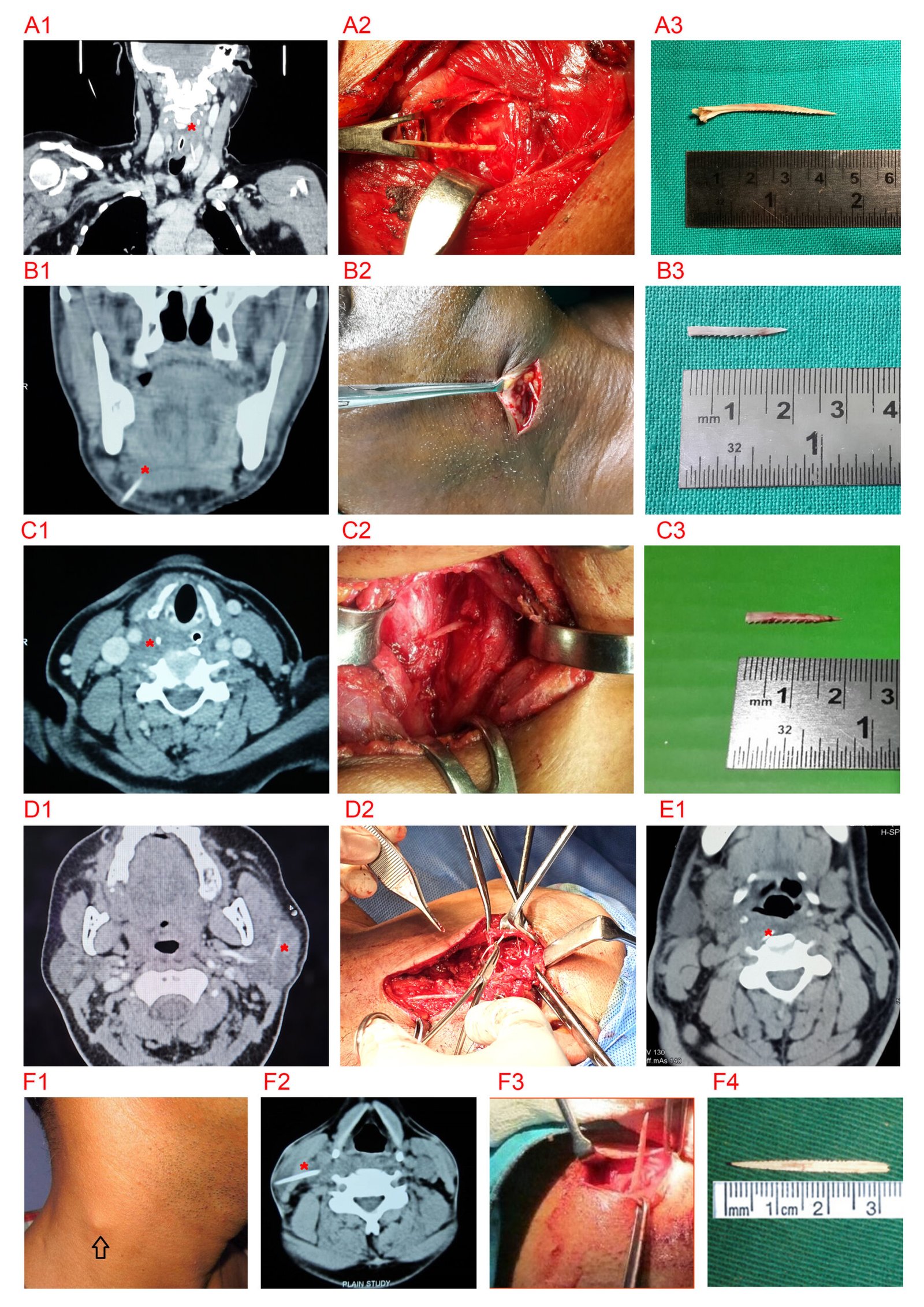
Foreign bodies in the upper aerodigestive tract are a common emergency in ENT practice. In most cases, these objects are promptly identified and removed using routine procedures like laryngoscopy or hypopharyngoscopy. However, a small subset of foreign bodies, particularly those with sharp edges, can breach the pharyngeal mucosa and migrate extraluminally into the neck spaces. This rare occurrence, termed “migratory foreign bodies,” necessitates precise diagnosis and surgical intervention.
Our Study: Key Insights
Our multicentric observational study, conducted across medical centers in India, analyzed 15 cases of migratory foreign bodies over several years. Patients ranged from 11 to 70 years of age, with symptoms varying from neck pain and dysphagia to more subtle presentations like pricking sensations in the throat. The most common culprits were fish bones, followed by chicken bones and metallic wires.
Diagnostic Challenges
One of the most critical aspects of managing these cases is diagnosis. While lateral neck radiographs provide initial insights, computed tomography (CT) scans proved indispensable in confirming extraluminal migration. These scans not only identified the location and type of foreign bodies but also guided surgical planning by mapping their relationship to vital neck structures.
Surgical Adventures
The retrieval of these foreign bodies often required meticulous surgical exploration. From the retropharyngeal space to the thyroid gland, parapharyngeal areas, and even the parotid duct, the sites of impaction were diverse. Intraoperative challenges, such as imprecise localization due to the mobility of neck structures, were mitigated by the use of intraoperative radiography.
Lessons Learned
Our study highlighted several key points:
- High Index of Suspicion: Migratory foreign bodies often present with vague or delayed symptoms. A thorough history and imaging are essential to avoid missed diagnoses.
- Early Intervention: Prompt recognition and surgical management can prevent severe complications, such as abscess formation or vascular injuries.
- Collaborative Efforts: Successful management requires coordination among radiologists, surgeons, and anesthetists to ensure optimal outcomes.
Why This Study Matters
To the best of our knowledge, this is one of the largest case series on migratory foreign bodies in otolaryngology practice. By documenting these cases, we aim to enhance the understanding of this rare condition and provide a framework for clinicians worldwide to manage similar scenarios effectively.
Looking Ahead
Our research underscores the need for continuous learning and adaptability in otolaryngology. Migratory foreign bodies remind us of the intricacies of the human body and the importance of a systematic approach to patient care. We hope this study serves as a valuable resource for clinicians and sparks further research in this fascinating area.
For more details, you can access our publication in the Journal of Laryngology and Otology here.
We are excited to share these findings with the broader medical community and look forward to engaging discussions and collaborations that advance patient care. If you have encountered similar cases or have insights to share, feel free to reach out to us!